Substance use disorders (SUD) are common among adolescents and young adults (AYAs) and cause lasting harms, including reduced cognitive function and altered neurobiology.1–3 Recent evidence suggests that SUD is more prevalent among AYAs with medical complexity, such as chronic physical, psychiatric, or intellectual/developmental conditions (henceforth “high-need AYAs”), than among their peers.4–8 For example, one study found that 51.7% of high-need AYAs report heavy substance use compared to 40.4% of AYAs without chronic conditions.5 Similarly, a Canadian study found that the prevalence of any SUD was higher among AYAs with chronic physical illness than AYAs without (2.4% versus 1.3%, respectively) with the exceptions of alcohol use and cannabis use.4 Understanding factors associated with the increased prevalence of SUD among high-need AYAs is particularly important, as there has been a call for increased research focus on this population due to their enhanced fragility relative to their peers.9 Additionally, both clinicians and families have identified behavioral issues such as substance use among this population as an important research objective.10 In North Carolina, addressing SUD has been identified as a focus of “Healthy North Carolina 2030,” a health improvement roadmap developed by the North Carolina Institute of Medicine for the state Division of Public Health,11 and advancing our understanding of SUD in this under-studied population is an important step toward identifying potential interventions to achieve the goal of reducing SUD.
In separate studies, older age and the presence of concurrent physical and mental health diagnoses have been shown to be associated with increased risk of SUD among high-need AYAs.4,7 Among the general AYA population, demographic (e.g., race) and environmental (e.g., neighborhood poverty) factors are associated with higher rates of SUD.3,12–15 Despite the prevalence and consequences of SUD among high-need AYAs, relationships between risk factors and the presence of SUD remain unclear. For example, questions remain regarding the role of insurance coverage, as many high-need AYAs are underinsured relative to their peers without high needs due to the expansive health care services often needed by this population.16 Additionally, it is unclear what role neighborhood-level opportunity has in the development of SUD in high-need AYAs, as this population is less likely to report community engagement (e.g., volunteering).17 Understanding these relationships is critical to shaping effective prevention, screening, and treatment efforts for SUD. Therefore, our objective is to identify the most significant risk factors associated with SUD among high-need AYAs in North Carolina.
Methods
Data and Participants
This retrospective cohort study was conducted using electronic health record (EHR) data from 2015 through 2019. Data were obtained from a large academic hospital system in North Carolina comprised of nine geographically dispersed hospitals. Patient records were geocoded at the census-tract level using the residential address to link neighborhood-level characteristics to patients. We used the Andersen Behavioral Model of Healthcare Use to select demographic, clinical, and environmental risk factors from the EHR.18,19 The Andersen Behavioral Model of Healthcare Use argues that health care utilization and outcomes are the result of predisposing (e.g., age), enabling (e.g., insurance), and need (e.g., complex medical conditions) factors, and it is widely used in health care research.18,19
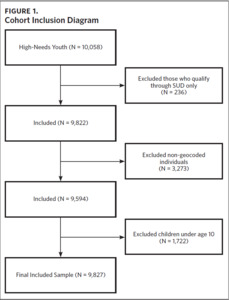
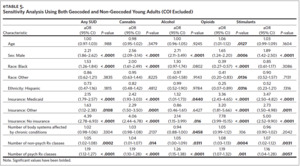
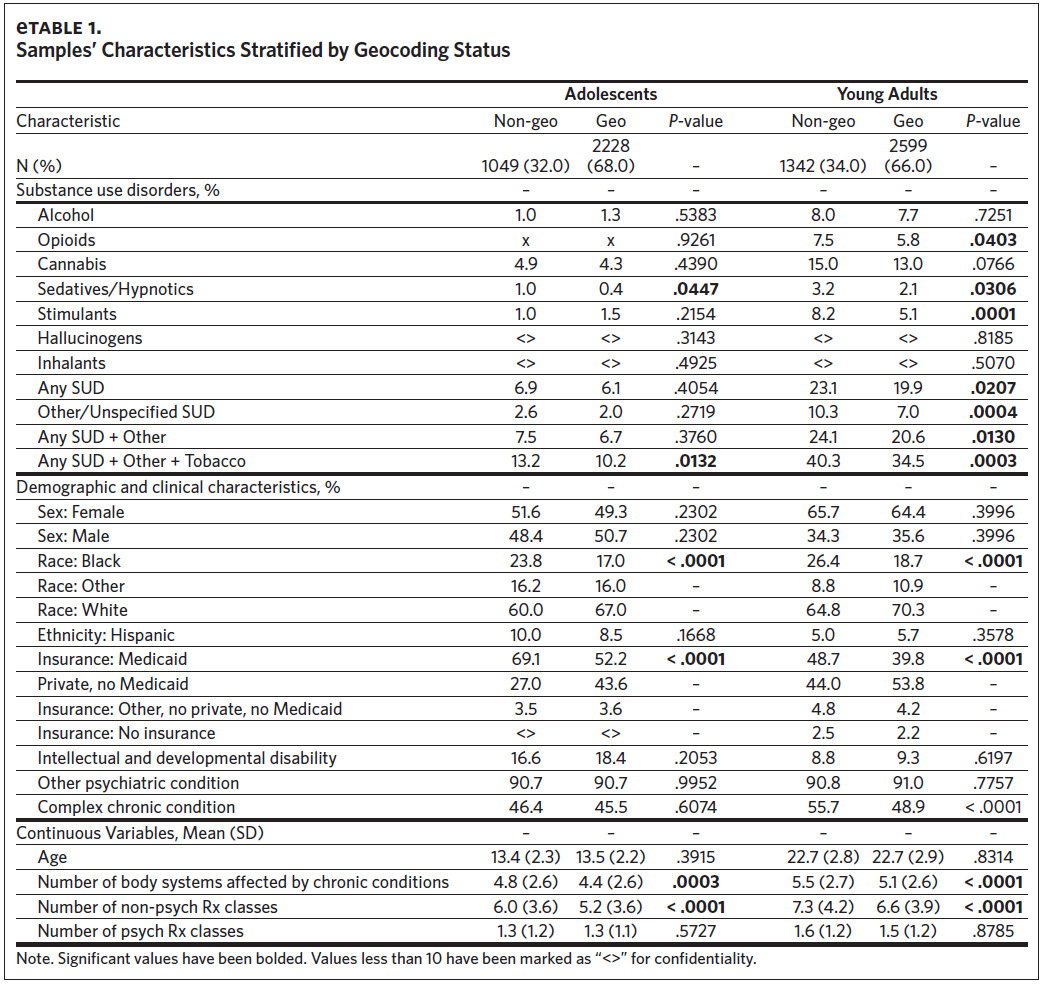
Cohort inclusion criteria were: 1) aged 27 years or younger at the first qualifying diagnosis; 2) having a qualifying condition for high medical needs based on ICD-9 and ICD-10 diagnosis codes using previously validated algorithms20,21; 3) at least two outpatient visits, one emergency department visit, or one inpatient hospitalization associated with the qualifying diagnosis during the study period; and 4) at least one encounter with the health care system annually. We used age 27 as the upper bound on our sample in order to cover the age at which children are no longer eligible for coverage through their parents’ insurance under the Affordable Care Act (age 26)22 plus an additional year for health care transitions to occur. Qualifying conditions included intellectual/developmental disorders, psychiatric diagnoses, and complex chronic conditions. We excluded those whose only qualifying condition was SUD (including nicotine), those missing a valid residential address, and children under age 10, resulting in a final sample of 4,827 (Figure 1). Given that a missing residential address potentially indicates transience, we examined differences in the characteristics of those with and without a valid residential address and identified several differences (Appendix eTable 1). This study was approved by the University of North Carolina at Chapel Hill Institutional Review Board.
Measures
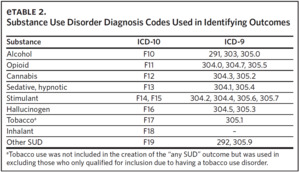
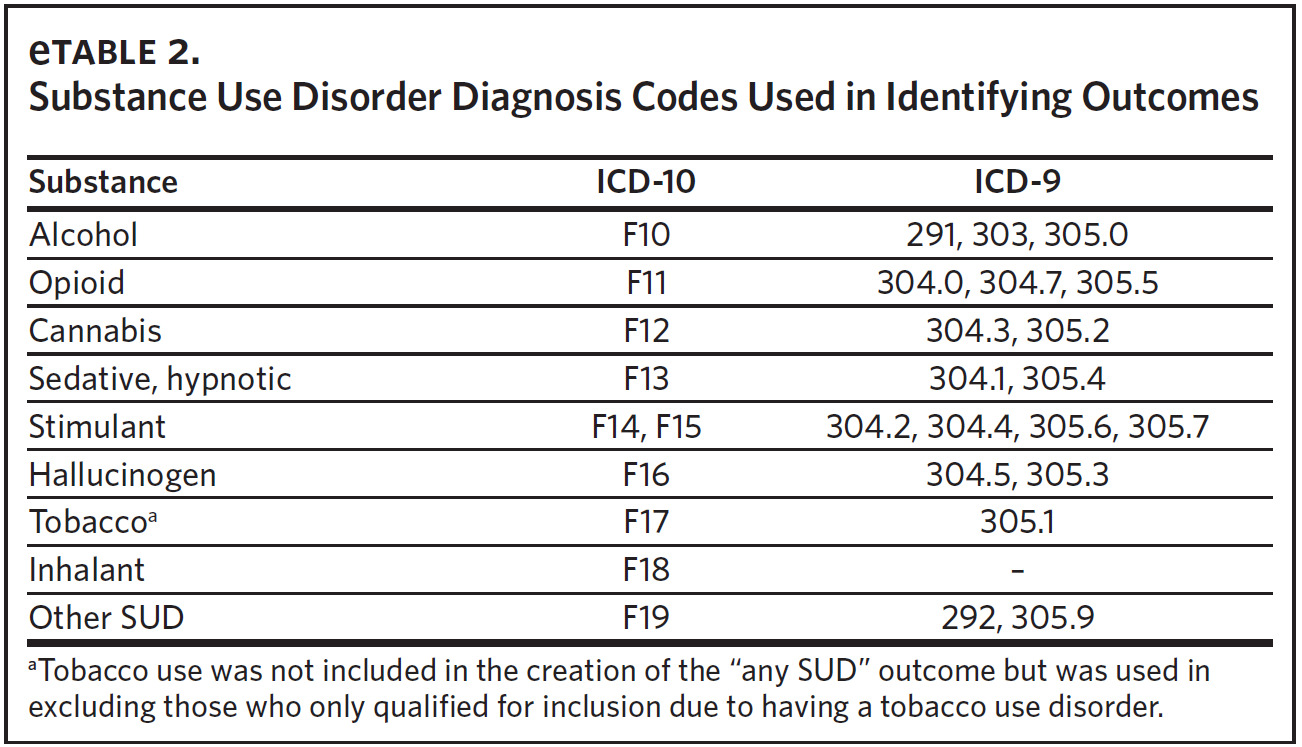
Substance use disorder. We identified the presence of SUD using ICD-9 and ICD-10 codes (Appendix eTable 2). Indicator variables were created for the following substances: alcohol, opioids, cannabis, stimulants, hallucinogens, sedatives/hypnotics/anxiolytics, inhalants, and other psychoactive substance-related disorders. An additional indicator variable was constructed to reflect the presence of any SUD. Nicotine dependence was not included in the creation of the indicator for any SUD given its unique nature relative to the other substances. We did not examine SUD stratified by severity (mild, moderate, severe) based on the expert opinion of the two clinicians on the study team.
Demographics and clinical factors. Demographic data included age, biological sex, race (recoded as White, Black, or Other), and Hispanic ethnicity. Given the range of ages included, we created an indicator variable differentiating adolescents (aged 10–17) and young adults (aged 18 or older) to facilitate stratified analyses. The social constructs of race and ethnicity are included as proximal measures of systemic racism and are not to be interpreted as biological differences.23 Insurance coverage was recorded as Private Insurance Only, Medicaid, Other (i.e., no private or Medicaid), and no insurance. The number of body systems affected by chronic medical conditions was identified using the Agency for Healthcare Research and Quality’s Clinical Classification Software.24 We also included the count of non-psychotropic medication classes prescribed and the count of psychotropic medication classes prescribed.
Child Opportunity Index. The Child Opportunity Index (COI) was developed to provide policymakers and health researchers with a summary metric for assessing neighborhood-level social determinants of health.25 We used the 2015 state-normed COI to capture environmental factors that could contribute to the risk of developing SUD.26 This measure produces a 29-item composite rating that describes the health/environmental (e.g., EPA walkability index), socioeconomic (e.g., median household income), and educational (e.g., high school graduation rate) opportunities available for each child at the census-tract level. The COI is an ordinal measure ranging from “very low” opportunity (a score of 1) to “very high” opportunity (a score of 5).
Statistical Analysis
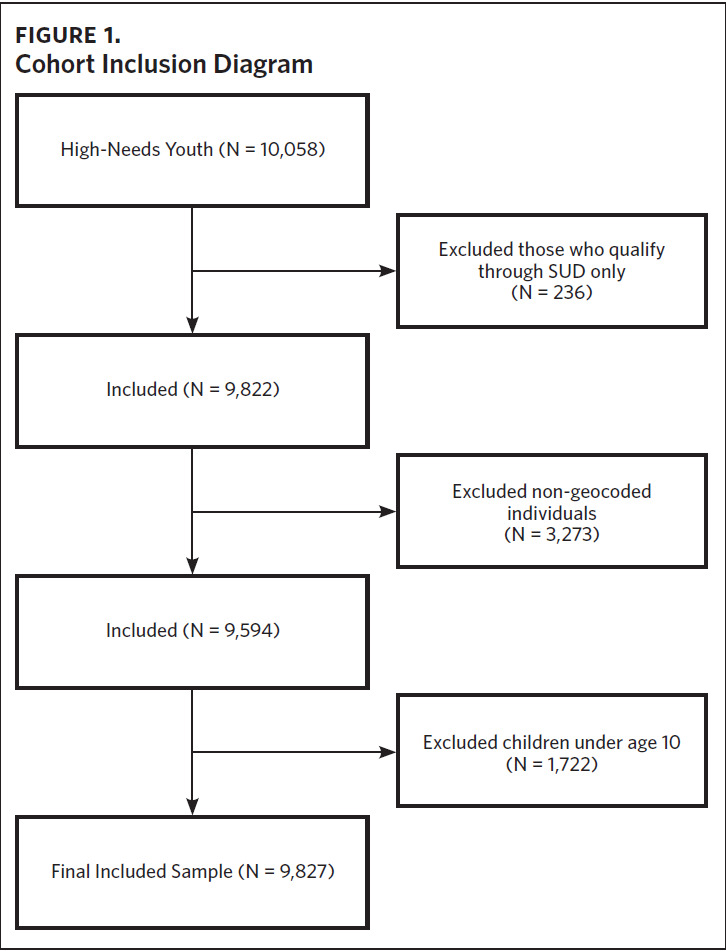
We examined descriptive statistics stratified by the presence of any SUD diagnosis and young adult status using chi-squared and t-tests. Associations between the risk factors and SUD were assessed using multilevel logistic regressions that included random intercepts for census tracts. Individual SUDs with less than 75 cases were not modeled due to concerns regarding precision and clinically meaningful findings. To examine the impact of excluding non-geocoded patients, we conducted a sensitivity analysis in which they were included, and the COI measure was dropped from the model. These results were compared to the main findings in terms of the direction of association (i.e., positive or negative) and the statistical significance of the estimates (i.e., whether a previously non-significant estimate became significant in the sensitivity analysis or vice versa).
Results
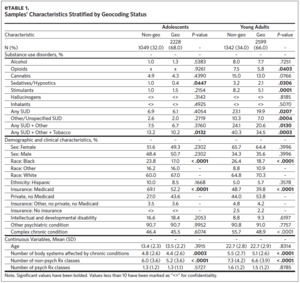
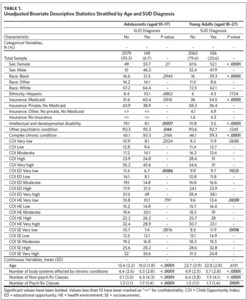
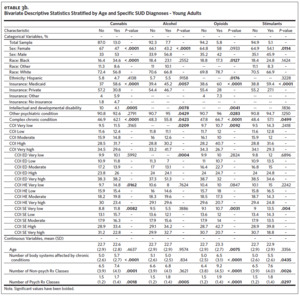
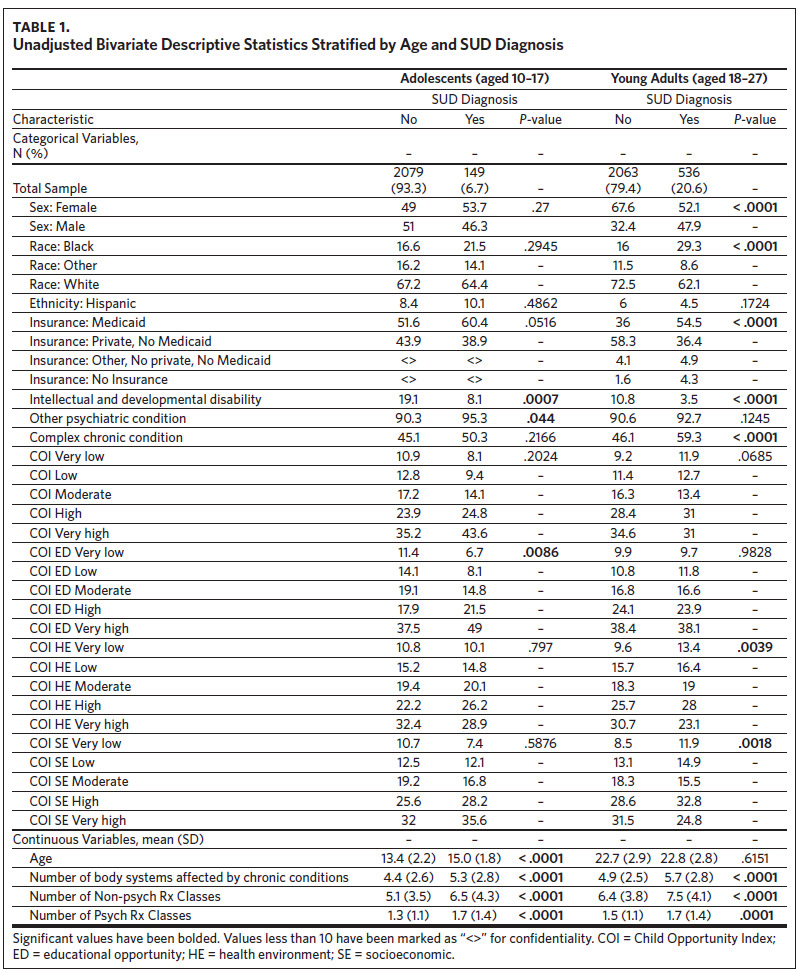
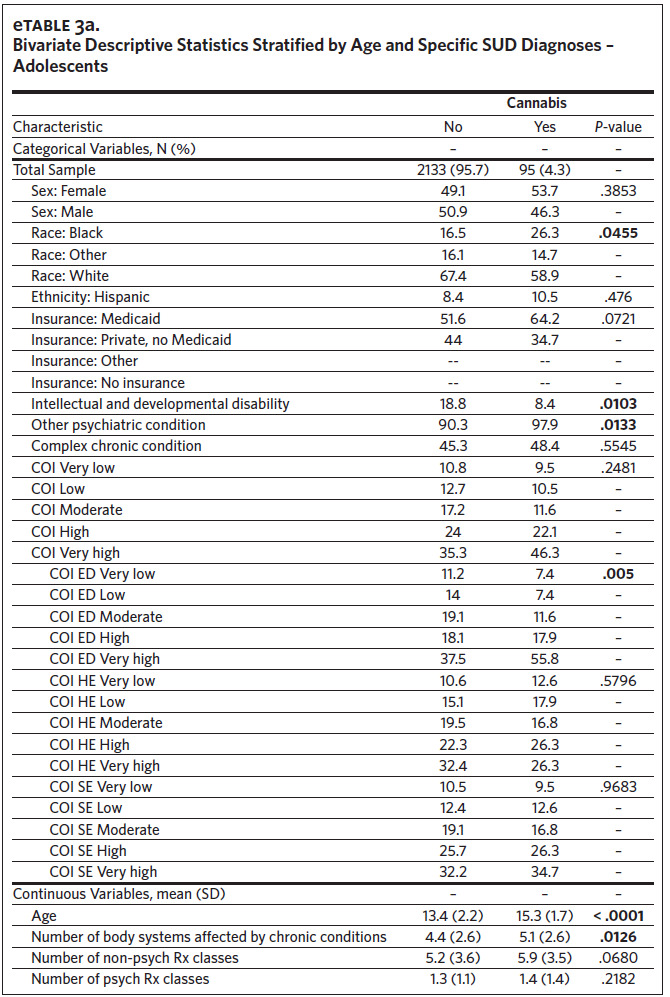
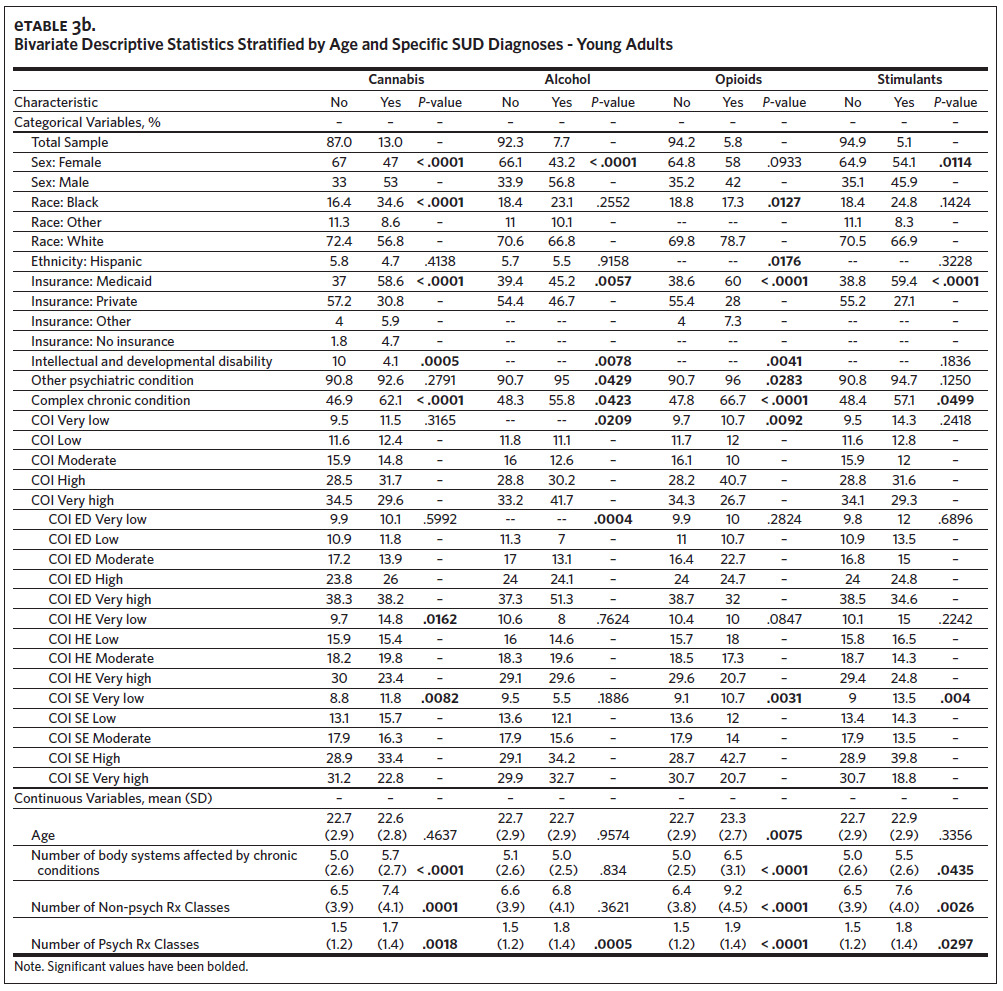
Our analytic sample (total N = 4,827) consisted of 2,228 adolescents (46.2%) and 2,599 young adults (53.8%) (Table 1). The subsample of adolescents had an average age of 13.5 (SD = 2.2) and was predominantly White (n = 1493, 67.0%), male (n = 1129, 50.7%), and insured through Medicaid (n = 1,162, 52.2%). The subsample of young adults had an average age of 22.7 (SD = 2.9) and was predominantly White (n = 1828, 70.3%), female (n = 1,673, 64.4%), and privately insured (n = 1,398, 53.8%). The overall prevalence of SUD was 14.2% (N = 685). There were 149 adolescents (6.7%) and 536 young adults (20.6%) with any SUD, with cannabis being the most prevalent qualifying SUD among both groups (adolescents: n = 95, 4.3%; young adults: n = 338, 13.0%). The prevalence of any SUD by age and COI can be found in Appendix eFigure 1 and eFigure 2, respectively. Among adolescents, the only SUD with a sufficient sample for individual analyses (n > 75) was cannabis (n = 95, 4.3%) (Appendix eTable 3a), while analyses of cannabis (n = 338, 13.0%), alcohol (n = 199, 7.7%), opioids (n = 150, 5.8%), and stimulants (n = 133, 5.1%) were possible among the young adults (Appendix eTable 3b).
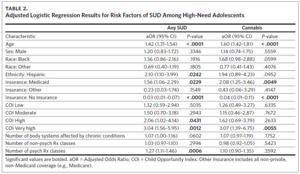
Factors Among High-Need Adolescents
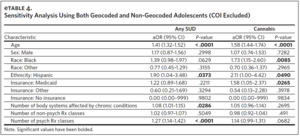
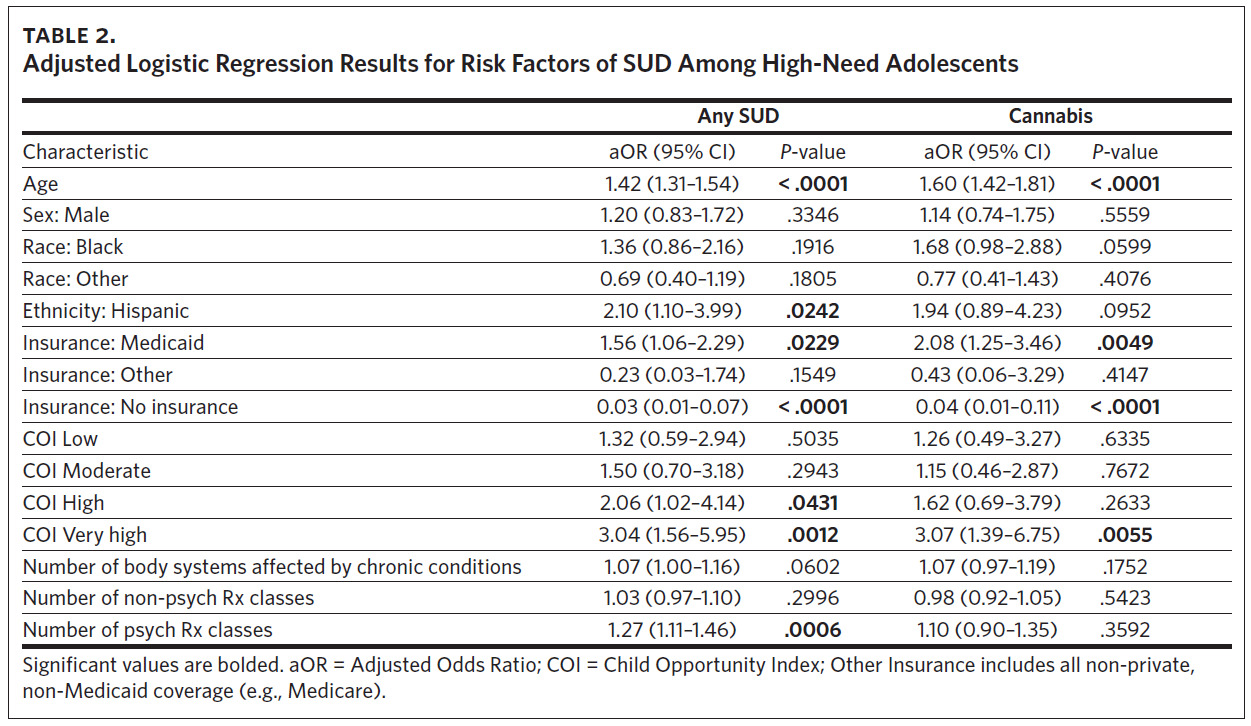
Our primary analysis identified several demographic, clinical, and neighborhood factors associated with the presence of any SUD diagnosis among the subsample of high-need adolescents (Table 2). Additional years of age (adjusted odds ratio [aOR] = 1.42, 95% CI = [1.31, 1.54]) and Hispanic ethnicity (aOR = 2.10, 95% CI = [1.10, 3.99]) were both associated with increased odds of having a SUD. Relative to adolescents with private insurance, those with Medicaid had 56% higher odds of having SUD (aOR = 1.56, 95% CI = [1.06, 2.29]) while those who were uninsured had 97% lower odds of having SUD (aOR = 0.03, 95% CI = [0.01, 0.07]). Neighborhood characteristics were indicative of SUD risk as well, with the “high” and “very high” COI categories having odds of SUD that were 106% and 204% higher than the “very low” COI category, respectively (high: aOR = 2.06, 95% CI [1.02, 4.14]; very high: aOR = 3.04, 95% CI [1.56, 5.95]).
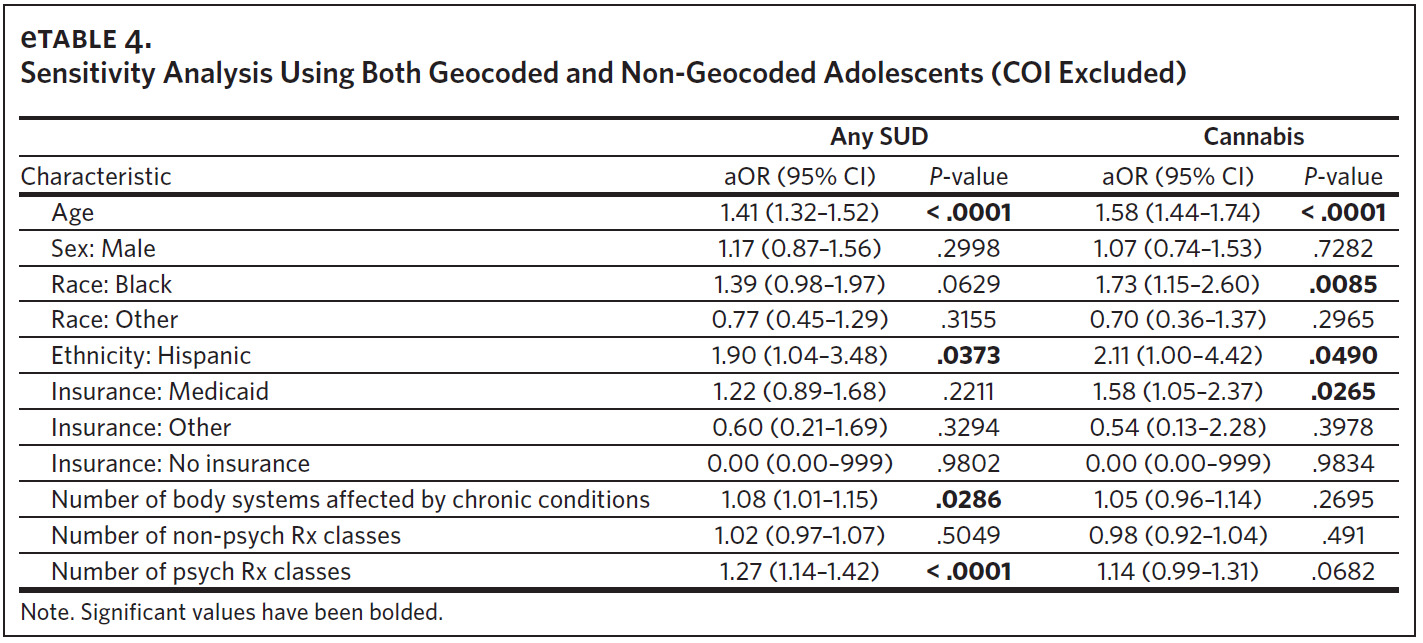
Finally, each additional psychoactive medication class prescribed increased the odds of SUD by 27% (aOR = 1.27, 95% CI [1.11, 1.46]). These results were robust in the sensitivity analysis (Appendix eTable 4). The risk factors for cannabis use disorder were nearly identical to those for any SUD, with the exceptions of Hispanic ethnicity, “high” COI, and the number of psychoactive medication classes, which were no longer significant (Table 2).
Risk Factors Among High-Need Young Adults
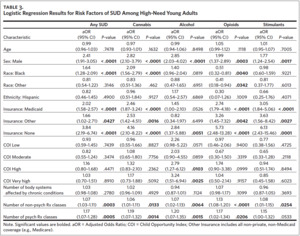
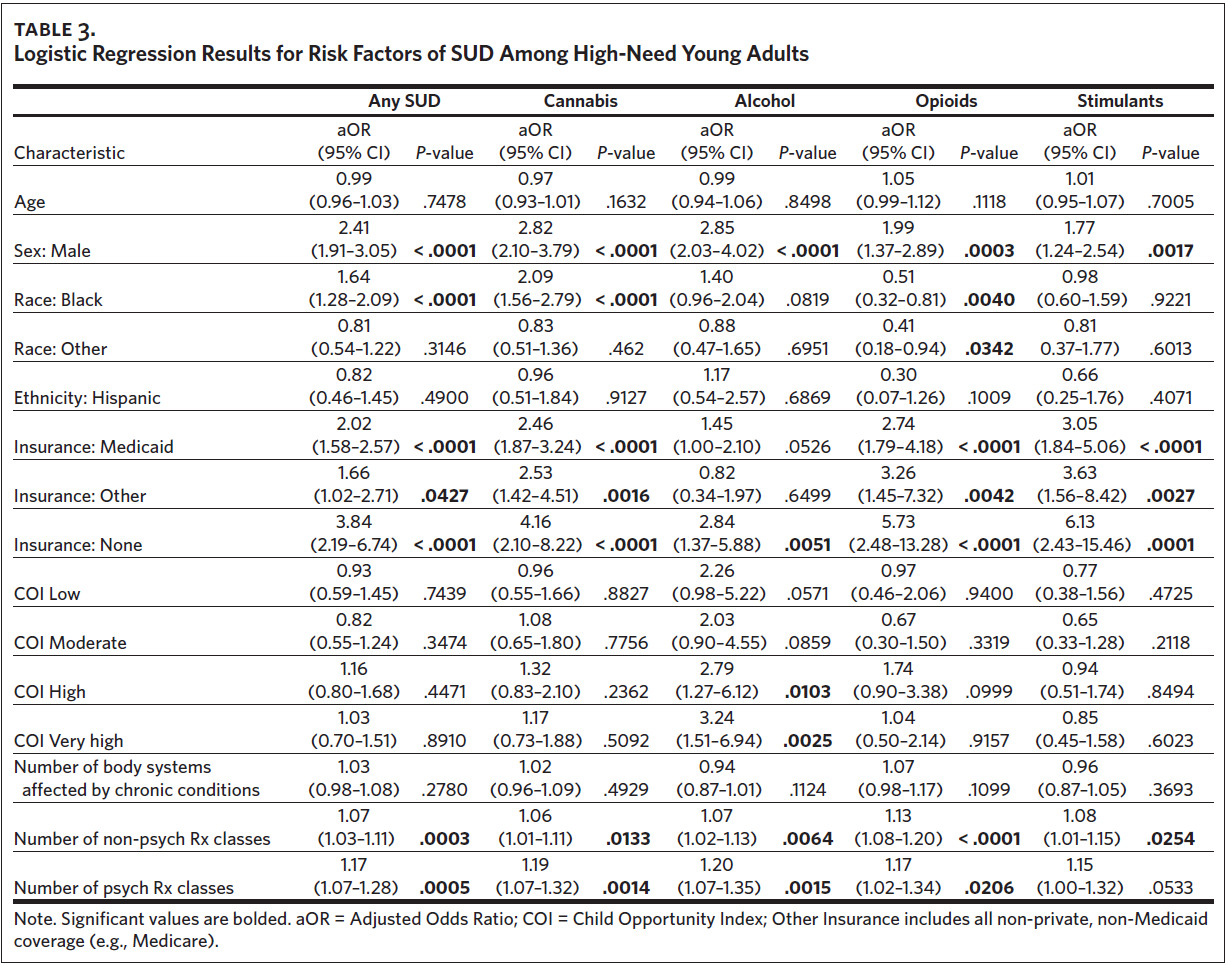
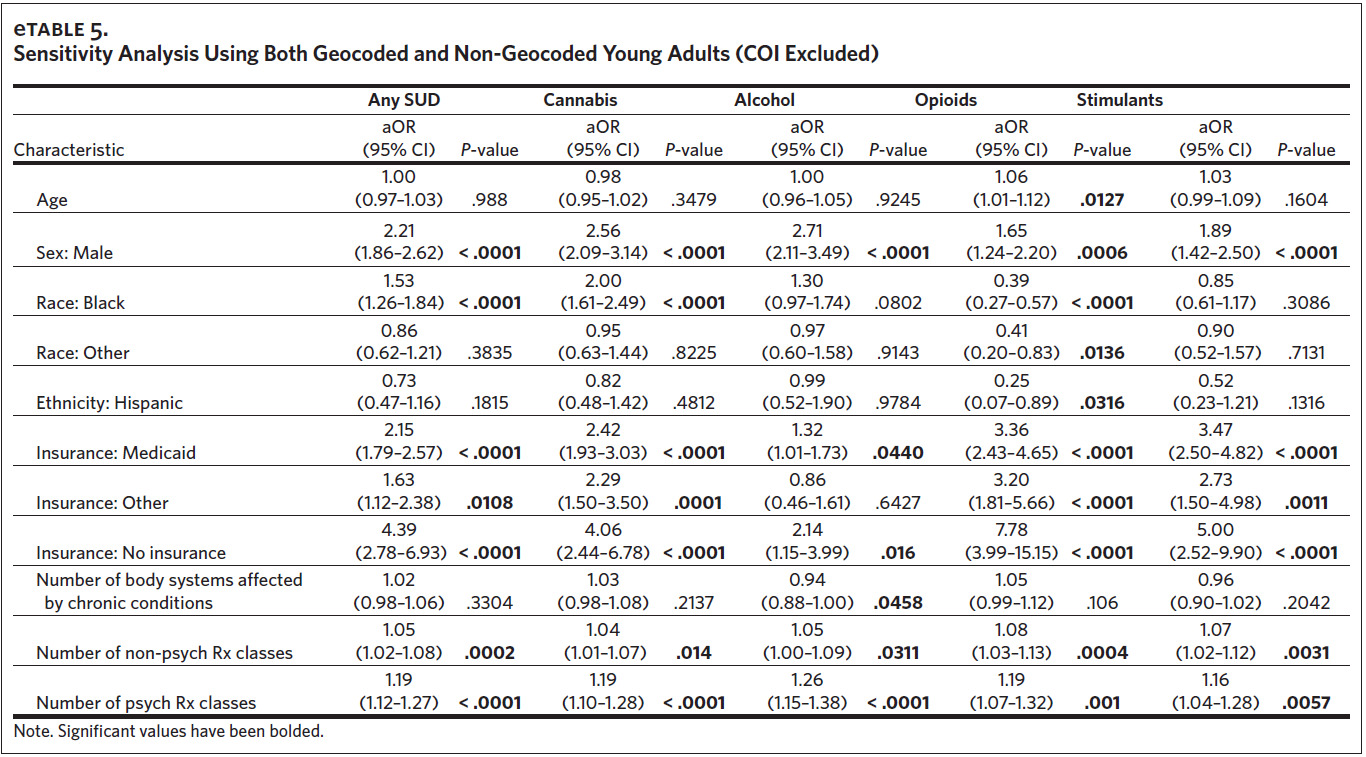
Among high-need young adults, we identified several risk factors for any SUD (Table 3), and these results were robust in the sensitivity analysis (Appendix eTable 5). The odds of any SUD were 141% higher among males than females (aOR = 2.41, 95% CI [1.91, 3.05]) and 64% higher for Blacks than for Whites (aOR = 1.64, 95% CI [1.28, 2.09]). Compared to private insurance, the odds of having SUD were higher for those with Medicaid (aOR = 2.02, 95% CI [1.58, 2.57]), Other Insurance (aOR = 1.66, 95% CI [1.02, 2.71]), and No Insurance (aOR = 3.84, 95% CI [2.19, 6.74]). Higher medication usage was also associated with higher odds of having any SUD. Each additional non-psychoactive medication class was associated with a 7% increase in the odds of SUD (aOR = 1.07, 95% CI [1.03, 1.11]), and each additional psychoactive medication class was associated with a 17% increase in the odds of SUD (aOR = 1.17, 95% CI [1.07, 1.28]).
The risk profiles for specific SUDs were generally similar to those for any SUD, with cannabis and stimulant use having identical risk factors (Table 3). For alcohol use disorder, the risk profile differed from that of any SUD in that there were no racial differences and no association with having Other Insurance. Additionally, young adults from “high” and “very high” COI areas had 179% and 224% higher odds of alcohol use disorder, respectively (high: aOR = 2.79, 95% CI [1.27, 6.12]; very high: aOR = 3.24, 95% CI [1.51, 6.94]). The risk profile of opioid use disorder was similar to that of any SUD with the exception of race. Compared to Whites, Blacks had 49% lower odds of opioid use disorder (aOR = 0.51, 95% CI [0.32, 0.81]) and other races had 59% lower odds (aOR = 0.41, 95% CI [0.18, 0.94]).
Discussion
We found that SUDs are prevalent among high-need AYAs at a level significantly higher than the general population of AYAs and at a level similar to several other relatively common conditions, such as asthma and depression. Among high-need adolescents, the prevalence of any SUD (6.7%) was nearly double that of the general population of adolescents (aged 12–17: 3.6%).27 The prevalence of SUD was also similar to the prevalence of attention-deficit/ hyperactivity disorder (7.2%)28 and asthma (8.3%).29 Among high-need young adults, the prevalence of any SUD (20.6%) was nearly triple that of the general population of young adults (aged 18–25: 7.5%),27 and similar to prediabetes (24.0% among people aged 19–34)30 and depression (21.0% among people aged 18–29),31 and was higher than symptomatic attention-deficit/hyperactivity disorder (8.99% among people aged 18–24, 8.27% among people aged 25–29).32 Given that the prevalence of SUD in this population is orders of magnitude larger than that of the general population and similar to several common conditions, it seems pertinent for providers to actively screen for SUD among high-need AYAs.
Our finding of increased SUD risk in high or very high COI areas for adolescents suggests that higher opportunity is not necessarily associated with lower risk among this population, as it is in the broader AYA population. For example, prior research demonstrated that attending a high-performing school was associated with reduced substance use,33 but our results suggest this may not be the case among high-need AYAs. We hypothesize that living in a high or very high COI neighborhood could provide increased access to recreational drugs (e.g., cannabis), which prior studies have demonstrated are sometimes used by high-need AYAs to self-medicate.6,8 However, there is little research on this issue, and future work is needed to better understand which components of neighborhood opportunity contribute to this relationship.
Limitations
This study had several limitations that may impact generalizability. First, this study was conducted using electronic health record data. While these data contain rich information about health and service use, there are concerns about truncation. For some patients, SUD diagnosis may not be observed if they received a diagnosis that occurred either prior to entering our data or after the five-year observation window. Similarly, it is possible that some AYAs had a SUD not documented in the data because it was either undiagnosed or was not coded in their health record for various reasons (e.g., substance use was discussed but not a primary diagnosis for the visit) as described in prior literature on electronic health records.34,35 This also raises the larger issue of the potential for variation in how SUD was diagnosed in these patients. While there are diagnostic criteria for SUD, we are unable to see the rationale for each diagnosis in our data.
Second, the exclusion of non-geocoded AYAs may have reduced the generalizability of our sample. The relevant sensitivity analyses provided evidence that the exclusion of these AYAs did not meaningfully alter our findings; however, their COI distribution (excluded for the sensitivity analysis) may have differed from the geocoded AYAs in a meaningful way. Missing geocoded data has been recognized as a common issue and potential source of bias in social determinants of health research.36
Third, it is highly plausible that the COI for young adults in our sample is not the one in which they grew up. While the COI is still informative for the young adults in that it describes their current neighborhood characteristics, it likely does not have the same impact as for adolescents. For this reason, the association between the COI and SUD should likely not be compared between adolescents and young adults.
Fourth, we did not include children under age 10 in our analysis; however, of the 1,722 children under age 10 that we excluded, a total of 10 children had a SUD diagnosis, including opioid, stimulant, and cannabis use. Future studies with larger samples should examine the prevalence of SUD among high-need AYAs in this population. Finally, the data in this sample come from a large academic hospital system in North Carolina and may not be representative of all high-need AYAs.
Clinical Implications
We found relationships between the number of medications prescribed and the presence of any SUD, suggesting that medications used to treat chronic conditions may themselves be risk factors for the development of SUD. This is consistent with prior studies that have demonstrated specific medication-SUD relationships, such as the higher risk of opioid use among people using asthma inhalers.37 The number of medications may plausibly represent a proximal measure of disease burden; however, given the inclusion of a disease severity measure, we hypothesize that this relationship reflects an added level of comfort with taking medications. We propose that medication use may become normalized among high-need AYAs receiving pharmacotherapy, resulting in the development of health beliefs that may generalize to non-prescribed substances. Additionally, increased prescribing of psychotropic medications in particular may provide opportunities for drug misuse.
A prior study found that high-need adolescents often adjust their medication regimen to accommodate substance use and sometimes use marijuana in place of alcohol in order to limit medication interactions.8 Given that both the familiarity with medications and the risk of medication interactions goes up with additional medications prescribed, AYAs with more medications may be more likely to use illicit substances and therefore be identified as having SUD. However, we caution that considerable future research is needed to support this hypothesized explanation before any definitive actions should be taken regarding this association. In particular, a study examining medication misuse and drug-related health beliefs in this population is needed to elucidate this association in order to develop clinical practices to address it. These findings do, however, underscore the need for clinicians and families to be particularly attuned to the potential for medication and drug misuse in high-need AYAs.
Public Health Implications
Broadly, our findings suggest a need to raise awareness about high-need AYAs and SUD among parents, caregivers, and providers. Prior work has found that there is a degree of awareness about the risk of SUD in patients with intellectual/developmental disabilities,38 but there is a need to explore this awareness regarding high-need AYAs more generally. In addition, it will be important to identify strategies for addressing current SUD among this population as well as the upstream drivers of SUD. There is some evidence that substance use in high-need AYAs is partially motivated by a perceived need for self-medication,8 suggesting that addressing unmet need for treatment may be a viable strategy for reducing SUD. However, considerable future research is needed to understand this issue more thoroughly. In particular, it is currently unclear how severe the problem of SUD in this population may be given the higher degree of medical complexity. Research describing the outcomes of high-need AYAs with SUD is needed for comparison to AYAs without high needs. It will also be important to study the health behaviors underlying the development of SUD in high-need AYAs to facilitate effective intervention development.
While not directly comparable, it is interesting to note that the demographic risk factors associated with SUD in our sample are generally consistent with unadjusted population prevalence estimates. For adolescents, we found that SUD was higher for those who are older and Hispanic, but no variation by sex. In the general population, the prevalence of SUD increases by age (0.8% at ages 12–13 to 6.1% by ages 16–17) and is slightly higher for Hispanic than non-Hispanic adolescents (4.2% versus 3.4%) but does not vary substantially between male and female (3.4% versus 3.8%).27 For young adults, we found that SUD was higher for those who are male or Black. The increased SUD we saw among males aligns with the unadjusted population estimates (males = 8.5%; females = 6.1%)27; however, the prevalence of SUD among those who are Black (7.2%) is lower than among those who are White (8.0%) in the unadjusted population prevalence estimates, diverging from our findings.27 While these comparisons to the general population should be considered cautiously due to the unadjusted nature of the population estimates, it is suggestive that these demographic differences in our findings may be reflective of population-level variation rather than being unique to high-need AYAs. Future research is needed to directly compare the predictors of SUD between high-need AYAs and the general population.
The differential risk of SUD by insurance status for young adults and adolescents raises several questions. Among high-need young adults, Private Insurance was associated with lower risk compared to Medicaid, Other Insurance, and No Insurance. Coverage by private insurance may reflect the availability of financial resources to treat SUD or more readily available health and mental health services to reduce the risk of SUD. However, there is considerable variation in private health insurance quality that is not captured by this categorization. Prior work among people with disabilities demonstrated that the adequacy of the network of providers covered by insurance is a stronger predictor of having unmet health care needs than the type of insurance.39 We hypothesize that this may be the case in high-need young adults as well, and this additional unmet need could potentially contribute to attempting to self-medicate. Future research is needed to examine this hypothesis; however, our findings suggest that increasing access to private insurance among high-need young adults may be a beneficial strategy. Among high-need adolescents, the relationship between insurance type and SUD was less clear, with Medicaid being a risk factor relative to private insurance. While being uninsured appeared to be associated with lower risk, we caution against over-interpretation due to the small number (n = 15) of adolescents who were uninsured. Future research is needed to explore the experience of insurance gaps among high-need adolescents.
Our finding that high-need adolescents from high and very high COI areas have a greater risk of SUD than others requires further research. The individual COI subscales (health, socioeconomic, and educational opportunity scores; Table 1) suggest that this relationship is driven primarily by educational opportunity. Among the general population of adolescents, factors included in the educational opportunity subscale, such as higher parent educational attainment and school quality, are associated with lower substance use.33,40,41 This incongruent finding among high-need adolescents suggests that there is a need for schools to focus on SUD prevention in this population. Future research is needed to better understand why a high COI—particularly educational opportunity—presents a risk factor for SUD among high-need adolescents.
Conclusion
Adolescence and young adulthood represent a period of increased substance use risk. This study of a large academic health care system in North Carolina found that the prevalence of SUD was high among a cohort of high-need AYAs and associated with several demographic, clinical, and neighborhood characteristics. These findings raise the need for future research to address prevention, screening, and treatment of SUD in high-need AYAs.
Declaration of interests
This research was partially supported by a National Research Service Award Pre-Doctoral/Post-Doctoral Traineeship from the Agency for Healthcare Research and Quality sponsored by The Cecil G. Sheps Center for Health Services Research, The University of North Carolina at Chapel Hill, Grant No. T32-HS000032.
Role of funder/sponsor
The funder/sponsor did not participate in the work.