Interprofessional education experiences are now an integral part of accreditation criteria for all health professional schools. While strong models exist for didactic interprofessional training, interprofessional practice opportunities are needed for students to apply the skills they learn in the classroom and simulation settings to real-world care environments.1–4 According to the National Collaborative for Improving the Clinical Learning Environment (NCICLE), the ideal interprofessional clinical learning environment (CLE) is a “shared space between various professions collaborating with patients and caregivers, working together to provide the best care possible” and can occur in any area where professional students are trained.5 Practice environments vary in the value placed on collaboration.6–9 The presence of different health care professionals does not automatically make an environment collaborative; it must be an intentional foundation of practice in that environment. Yet, assessment of the readiness and development needs of these CLEs to provide optimum interprofessional experiences remains underdeveloped.
With these needs in mind, the Interprofessional Clinical Learning Environment Assessment and Reflection (IP-CLEAR) tool was developed by a team of faculty from the schools of nursing, pharmacy, and medicine at the University of North Carolina at Chapel Hill (UNC-CH), with the support of the North Carolina Area Health Education Centers (NC AHEC) and the UNC-CH Office of Interprofessional Education and Practice (IPEP). The IP-CLEAR tool is intended for use by clinical sites that have or want to have clinical learners engaged and integrated into an excellent interprofessional CLE. The development of the IP-CLEAR and projections for future work are described here.
IP-CLEAR Tool Development
There have been two phases of development of the IP-CLEAR so far: information gathering and piloting testing. During phase one, a literature review determined the existing barriers to interprofessional collaboration in practice and methods used in assessing organizational readiness. The primary goals of IP-CLEAR were set as 1) categorizing the type of clinical site and infrastructure, 2) determining the existing degree of interprofessional collaboration, and 3) understanding the potential opportunities for interprofessional learners to engage. Two existing tools also served as foundational to initial tool development: the University of Minnesota’s Interprofessional Education Site Readiness (InSITE) tool and the Assessment for Collaborative Environments (ACE-15) tool.9,10 It was determined that an integrated, updated version of the tools may best meet the goals outlined. Content validity testing was conducted through semi-structured interviews, and after qualitative analysis themes were summarized to create the IP-CLEAR tool for pilot testing using the Qualtrics platform (Qualtrics LLC).
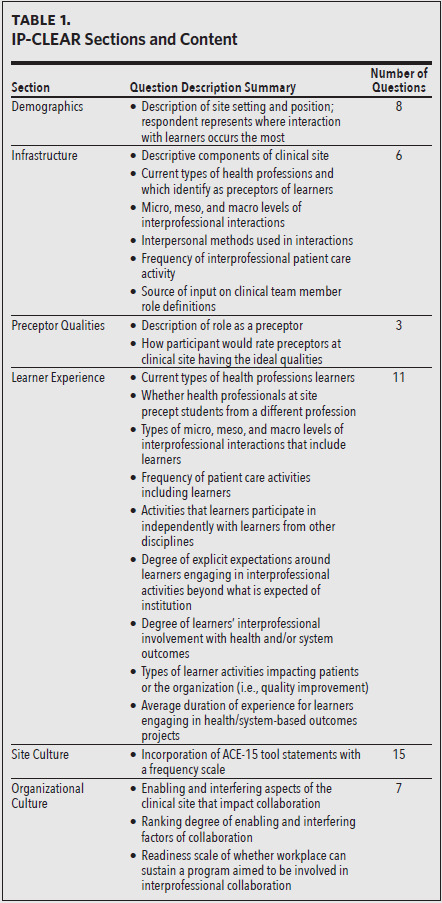
The IP-CLEAR tool contains six sections of items addressing demographics, site infrastructure, preceptor qualities, learner experiences, site culture, and organizational culture, with the section titles other than demographics borrowed from the InSITE tool. The IP-CLEAR tool differs in significant ways from its predecessors. IP-CLEAR incorporates defining the organizational levels of areas where multiple health professionals currently interact (such as at the unit or service level versus the entire clinic or hospital), as well as in-depth questions about learner experience. It also captures any additional involvement in projects related to health and system-based outcomes, and the section on site culture was based on the ACE-15 statements but used a frequency scale rather than an agreement scale to capture “team-ness” beyond a single moment in time.
During the pilot period of April–July 2022, individuals from clinical sites were asked to either independently complete the IP-CLEAR or schedule a 30-minute meeting with a project team member to complete it. The two types of administration processes were meant to assess the feasibility of IP-CLEAR completion. Sixty-four health professionals in North Carolina were contacted to complete the IP-CLEAR, 40 of whom started it and 23 of whom fully completed it. The clinical sites were from nine counties and from both inpatient and outpatient environments. Most respondents had mixed professional roles with administrative titles and backgrounds in either nursing, pharmacy, or medicine. Follow-up interviews were conducted to obtain feedback on the feasibility of administration of the IP-CLEAR. The feedback indicated that the IP-CLEAR is comprehensive and that, for feasibility, having a designated tool administrator was preferred to self-administration given the greater degree and depth of responses and their familiarity with interprofessional terminology to clarify any questions.
Next Steps
The overall goals for the development of the IP-CLEAR were met, and it will undergo further testing and refinement in future work to include demonstration of construct validity, assessment of inter-rater reliability among clinicians at one site and, ultimately, assessing the current structure of CLEs across more of North Carolina. A coaching model is being developed for clinical sites to address specific needs identified by the IP-CLEAR tool, with the goal of creating an action plan.
By improving clinical site evaluation through the development of a formative assessment tool, the hope is to provide information that can be used in assessing and improving the preparation of learners in collaborative practice. If you have a desire to be a part of this impactful work going forward, please consider contacting the UNC Office of Interprofessional Education and Practice at unc_ipe@unc.edu.
Acknowledgments
The authors want to acknowledge the work of Sofia Aliaga, Archana Sangamanarayanan, Stephanie Caruso, and Emili Anderson, without whom this project would not have been possible.