Asian immigrants make up a significant portion of North Carolina’s foreign-born population, second only to Latines.1 Despite pervasive images of Asian immigrants as affluent, highly educated, and self-sufficient, many Asian communities in the United States, such as Southeast Asian refugees, have experiences that do not align with “model minority” myths.2 Compared to their voluntary Asian immigrant counterparts, Asian refugees have, on average, lower levels of education, lower English language proficiency, higher unemployment, and higher levels of pre-migration trauma.3 Additionally, Asian refugee populations are frequently underserved by our social and medical systems, impacted by major barriers to care and higher burdens of negative health outcomes compared to the general US population.4
The Karenni are an example of one underserved Southeast Asian community. The Karenni are an Asian ethnic minority, originally from the Karenni State, whose persecution by the military regime in Myanmar (also known as Burma) led to their status as refugees and internally displaced persons (IDP).5 Since resettlement began in 2009, nearly 1,500 Karenni now live in North Carolina, with an estimated 800 adults and children living in Forsyth County (H. Meh, personal communication, May 17, 2023). Little is known, however, about the health needs or priorities of Karenni refugees in the United States. The purpose of this assessment was to detail the health needs and priorities of the Karenni community in Forsyth County.
Methods
A mixed-mode survey (i.e., online and in-person) was utilized to assess community health needs, health and public health service utilization, and social determinants of health for the Karenni refugee population living in Forsyth County, North Carolina.
Survey questions were developed through a collaboration between a representative from a local community organization, the Karenni Community of Winston Salem (KnC of WS), and a researcher at the Wake Forest University School of Medicine. The Karenni community partner, who also leads the public health committee of KnC of WS, originated the idea of a community needs assessment and recruited the Wake Forest University School of Medicine partner for collaboration.
The survey consisted of three main parts: sociodemographics, health care and public health service utilization (e.g., sources of health care, sources of health knowledge, and barriers to health care), and community health and needs (e.g., community priorities, concerns, and sources of community strengths). Sociodemographic information was collected via close-ended multiple-choice questions while open-ended questions were utilized to facilitate richer, detailed responses about community health and needs. Data about health care and public health service utilization were collected using both close-ended (e.g., When you get sick, where do you go?) and open-ended questions (e.g., What barriers/challenges prevent our community from using health care services?). Before distribution, the survey was pilot tested with three Karenni community members of various ages (i.e., aged 23 years, aged 30 years, and aged 65 years); changes for clarity and brevity were made to the survey based on their feedback.
Eligibility criteria for the survey included being aged 18 years and older, identifying as Karenni, and living in Forsyth County. Survey data were collected using a combination of online and in-person surveys. An anonymous Qualtrics survey was distributed via a Karenni community group chat; those who were eligible were encouraged to take the survey and share the link with their networks. This survey was self-administered, offered in English and Burmese, and took roughly 15 minutes to complete.
Additionally, data were collected using in-person interviews to reach adults who were uncomfortable using an online survey or who had low proficiency in written English or Burmese. Survey administrators would visit Karenni households to recruit participants. After the researchers confirmed eligibility, the survey administrator would read each survey question aloud in Kayah and record the participant response in English. Only survey staff and interview participants were present during the interview. In-person data collection visits took about 30 minutes to 1 hour.
Our team collected data during March 2023, with a total of 101 responses. Of the 101 individuals surveyed, we collected data from 36% (n = 36) using the online survey and from 64% (n = 65) using in-person data collection methods.
Although not conventional, five of the in-person surveys were completed as group interviews, each of which included the perspectives of 15 unique Karenni adults. This strategy was culturally appropriate, aligning with Karenni values of theh plaw theh jie, or togetherness, and allowed the assessment team to hear from more hard-to-reach members of the community. In these group interviews, we collected responses to qualitative questions (e.g., community priorities and concerns, barriers to care), from all participating adults while demographic information (e.g., education and employment status) was collected from a single participating survey respondent.
We described quantitative measures descriptively using counts, percentages, and range. Whenever possible, these results were compared to state and national data.1,6,7 Qualitative responses were analyzed using constant comparison and summarized into themes.8
Results
Sociodemographics
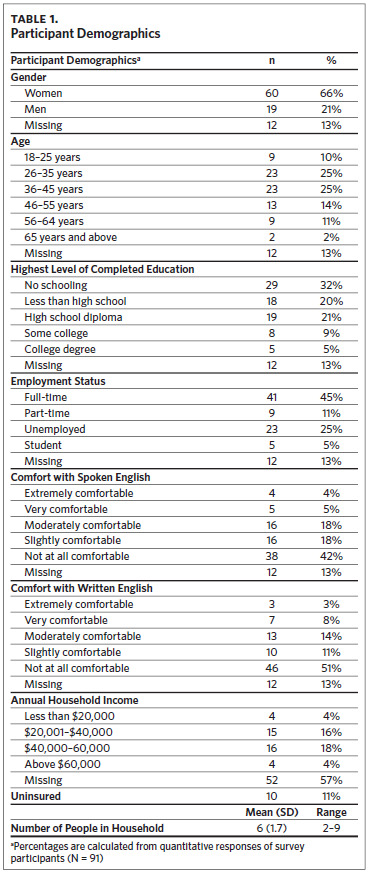
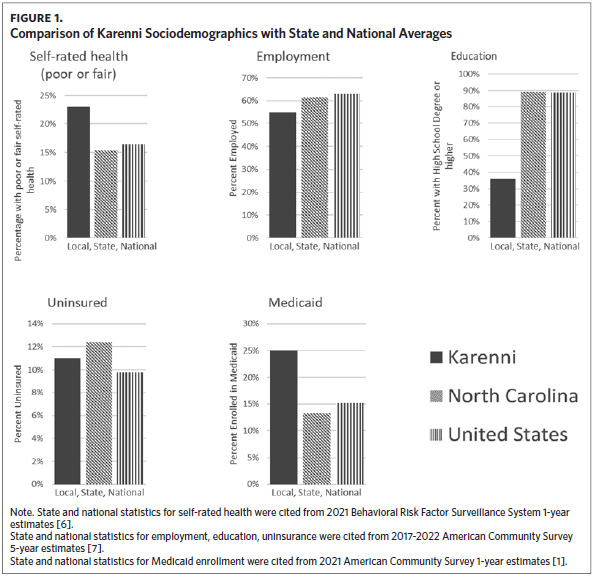
Detailed demographics for the surveyed Karenni can be found in Table 1 and Figure 1. More than half (60%, n = 55) of those surveyed had lived in United States for more than 10 years, with the majority spending the entire time as residents of Forsyth County (46%, n = 42). Compared to state and national statistics, a lower proportion of the Karenni community of Forsyth County have a high school education (35%; n = 32) or are employed (55%; n = 50).7 Proportions of poor or fair self-rated mental health (23%; n = 21) and those with Medicaid coverage (25%; n = 23) are also higher than state and national averages; the proportion of uninsured Karenni (11%; n = 10) is lower than the state average but higher than the national.1,6,7
Additionally, there were very low levels of English proficiency among the Karenni in Forsyth County. All survey participants listed Kayah as their primary language, and only 9% reported being extremely or very comfortable with written (n = 10) or spoken English (n = 9).
Health Care Utilization and Identified Barriers
Participants listed several barriers to health care and reported relatively little utilization of preventive care or well visits; a lack of check-ups and regular care were prevalent qualitative themes through the surveys. Participants reported that the greatest barriers to accessing health care were language and cost. Participants rarely had access to in-person interpretation, and barriers to remote interpretation include long wait times and mismatches in dialect or language between interpreter and patient (e.g., health care workers may provide a Burmese interpreter instead of a Karenni interpreter; a Karenni interpreter may speak a dialect of Karenni not understood by the patient).
In addition to these barriers, participants also reported a lack of knowledge about the health system and medical procedures in general. Specifically, many reported not knowing how to apply for health insurance or how to use the insurance they had. This limited knowledge hindered health care utilization while also contributing to a fear of medical systems.
When health care was utilized, reactive sources of care were most common, with the emergency department as the most reported source, serving 22% of the participants (n = 22), followed by urgent care (18%; n = 18). Doctors/physicians, friends, family, the internet, and the workplace were all listed as sources of health information and education.
Public Health Service Utilization
Seventy-nine percent of participants (n = 72) reported having heard of the Forsyth County Department of Public Health (FCDPH); however, the vast majority of those either never (17%; n = 15) or rarely (44%; n = 40) utilized FCDPH services. Of all FCDPH services, the immunization program was the most widely used (56%; n = 57) as the health department provided the required health screening and immunizations for refugee resettlement. Some continue to use this program for flu and COVID-19 vaccinations. The Women, Infants, and Children (WIC) program was the second most used program (34%; n = 34).
Community Priorities and Concerns
Mental health (32%; n = 29), chronic pain (18%; n = 17), and health care access (described previously) (29%; n = 26) emerged as priorities when respondents were asked about the most important health issues in the community. Conversations relating to mental health occurred across all data collection modes and in all age groups (except for age 65 years and older), with the highest proportions of discussion occurring among those aged 26–35 (present in 57% of discussions amongst that age group; n = 13) and 36–45 (present in 30% of discussions; amongst that age group; n = 7). Concerns about depression, anxiety, and stress were frequently discussed, and often situated in the context of past trauma, generational gaps between refugee parents and US-born children, and women’s health (i.e., postpartum depression). Commonly reported coping mechanisms for mental health concerns include excessive drinking and gambling. Online responses provided the most in-depth discussion of mental health, followed by in-person solo interviews and in-person group interviews.
Types of chronic pain, including headaches and back, arm, and knee pain, were also commonly discussed. Concerns about physical pain were attributed most often to mental health concerns (e.g., “anxiety and stress lead to physical aches”) or work (e.g., “chronic body pain from long time work and even after stopping working”). Participants shared that due to limited English skills and no formal schooling, many could only work at manual labor jobs with limited opportunities for career advancement or career growth. According to respondents, this manual labor also contributed to many of the chronic pain and vision problems impacting Karenni working adults.
To address the priorities above, particularly mental health and lack of health care access, participants expressed the need for health education and other promotion programs developed for Karenni needs. They suggested trainings to dispel stigmas that “associate mental health with demonic possession” and to help community members “learn how to let go of our emotions in a healthy way,” as well as education to help the Karenni better navigate American health care systems.
Community Strengths
Participants highlighted collectivistic cultural values and local community organizations as strengths of the Karenni community. Theh plaw theh jie, or “togetherness,” was the most reported strength in the survey. Community support and sense of belonging strengthened ties between Karenni families as they navigated shared challenges related to life in refugee camps and resettlement in the United States. Karenni community connectedness continues in North Carolina among the local residents (e.g., provision of instrumental and emotional support for community funerals) and is extended to other Karenni communities outside the country (e.g., fundraising events to support Karenni IDP in Myanmar after the 2021 military coup).
Participants also cited community organizations as a strength of Forsyth’s Karenni community. The local Winston- Salem community has established a community organization, KnC of WS, to support local Karenni affairs; KnC of WS includes elected leaders and 10 committees, one of which is devoted to public health. The organization is also connected to national organizations such as the Karenni-American Association (KnA). Businesses and faith-based organizations also emerged as sources of community strength, including the Calvary Baptist Church, which ordained the nation’s first Karenni pastor.
Discussion
These results characterize the Karenni community of Winston-Salem, North Carolina, as an underserved community with significant health needs and barriers to health care. Individual and contextual barriers to care include limited English proficiency (LEP), a lack of health education, limited language access services, and social determinants of health (e.g., lower levels of education and employment and higher enrollment in Medicaid than state and national averages). These findings also indicate potential points for intervention. To improve health care access and health outcomes for this refugee population, North Carolina providers and public health practitioners should partner with community organizations, a frequently cited source of community strength, to create multilevel interventions addressing priorities set by the Karenni.
Interventions should address systematic barriers to health care, such as a lack of Karenni interpreters and limited access and understanding of health insurance. The proportion of Karenni adults with LEP (82%; n = 75) is nearly twice as high as the statewide statistic of Asian American LEP adults (44%)1; additionally, Asian Americans with LEP have lower odds for preventive care, lower odds for having a usual place of care, and higher odds for unmet medical needs and communication issues.9 Unfortunately, there is only one professional in-person Karenni interpreter currently in Forsyth County and options for Karenni remote interpretation are extremely limited. Access to professional interpreters has been associated with improved clinical care, particularly for LEP patients, underscoring its importance in mitigating health and health care inequities.10 While remote interpretation can help fill in language gaps, in-house interpreters were considered more desirable by the survey respondents and help decrease wait times for vulnerable patients. Even when surmountable language barriers are addressed, limited community understanding of health insurance, concerns about cost, and a lack of familiarity with US health care serve as significant obstacles to care.
Respondents also indicated significant concerns about mental health and chronic pain. Due to traumatic experiences throughout pre-migration (e.g., war, persecution, murder), time spent in refugee camps, and resettlement (e.g., language barriers, acculturation challenges, loss of social support),11 Southeast Asian refugees like the Karenni have a high prevalence of negative mental health outcomes, such as depression, anxiety, and post-traumatic stress disorder (PTSD), with point estimates ranging from 36% to 40%.4,11,12 Due to its stigmatization in Karenni culture, it is notable that mental health appeared as a priority across all data-collection modes and nearly all age groups. The increased amount of detail in the online responses, compared to in-person interviews, may be related to the greater anonymity of those who chose to take the survey remotely. Additionally, the Kayah language does not have as many words related to mental health as the English language (H. Meh, personal communication, September 9, 2023), which may have also limited the detail of in-person Kayah interviews.
Chronic pain is also highly prevalent among refugees, including those from Southeast Asia4,13,14; however, there is a relative dearth of interventions targeted toward refugees for these outcomes. Among interventions that do exist, multidisciplinary interventions appear effective in addressing pain intensity, physical function, and psychological health.15 Although mental health and chronic pain were prominent concerns, most Karenni do not access or receive health services due to the barriers to health care previously described.
Based on the results of this survey, community-based participatory approaches to research and intervention development have the potential to produce effective, culturally relevant, and acceptable programs for the Karenni community. Community-based participatory research (CBPR) can and has been used to develop more efficacious interventions and improve the cultural relevancy, quality, and dissemination of research studies.16–19 Additionally, CBPR partnerships have been used to successfully address health inequity and build community capacity among similar Southeast Asian refugee populations, such as the Montagnard and Khmer communities.20–22 This approach aligns with Karenni cultural values of theh plaw theh jie and could harness sources of community strength, such as trusted community and faith-based organizations, to inform development, implementation, and dissemination. For example, CBPR could be applied to evaluate an intervention that trains local Karenni community members as health navigators and/or to develop health education programming. This would help build community capacity, address barriers to care and community needs highlighted in the qualitative themes of the assessment, and produce culturally targeted health promotion and education, a strategy endorsed and found acceptable by survey respondents.
Limitations
This study used convenience sampling of Karenni refugee adults living in Forsyth County, North Carolina, thus, individuals agreeing to participate in the study may be different from those who declined. A review of the literature, however, demonstrates that thematic results in this survey were similar to issues impacting other Southeast Asian refugee populations (e.g., mental health, chronic pain, and barriers to care). A relative dearth of information about Karenni refugees in the United States limits our ability to determine if the Karenni community in Forsyth County is similar demographically to other US Karenni communities; however, a comparison to a community profile published about Karenni in Omaha shows similarities across low language access and utilization of health care.23 This limited amount of information about Karenni in the United States, however, demonstrates the importance of the data above and the need for more research about this community. Lastly, the majority of survey participants (and those who declined to participate) were unfamiliar with the concept of research, which served as a barrier to recruitment. Future efforts to engage the Karenni community should include efforts to increase education and awareness about research, including its purposes, its benefits, and its risks. Lastly, the survey was limited by missing data, with higher missingness found for qualitative questions (highest missingness: 20%) and sensitive questions regarding income (missingness: 57%).
Conclusion
Results characterize the Karenni as an underserved refugee community in North Carolina experiencing health and health care inequities. Concerns related to mental health, chronic pain, and health care utilization were pinpointed as community priorities. Barriers to health care and public health service utilization originated from many sources including limited knowledge of health care systems and social determinants of health (e.g., high levels of limited English proficiency). The survey also highlighted sources of community strength, such as theh plaw theh jie (i.e., togetherness) and trusted community organizations. Public health and health care systems should partner with the Karenni community to address community priorities and mitigate health and health care inequities.
Acknowledgments
We thank the Karenni Community of Winston-Salem (KnC of WS), Forsyth Department of Public Health, and all survey participants for their support and engagement during this project.
Disclosure of interests
The authors have no competing interests or funding to declare.