Introduction
Acentra Health provides cloud-based claims processing and care management products and services to 45 state Medicaid programs and 25 federal agencies spanning 12 departments. Our commitment to advancing health care outcomes nationwide includes the responsible integration of artificial intelligence (AI). AI applications range from diagnostic support in care delivery to comprehensive management of patient records and claims. This integration promises improved efficiency with higher accuracy and patient satisfaction. However, as AI technologies evolve, they bring forth both challenges and opportunities that must be addressed to harness their full potential.
Applying AI to Care Management and Claims Administration
AI is revolutionizing care management and health care administration by streamlining complex, repetitive tasks, enhancing decision-making processes, and enabling health care providers to focus more fully on patient care. Below, we explore specific use cases of AI applications at the beginning, middle, and end of the care management process, encapsulating intelligent document processing (IDP), document completeness checking, and correspondence generation.
Intelligent Document Processing
The IDP sequence utilizes AI to streamline the handling of large volumes of documents critical to health care management and claims administration. This process includes:
Document ingestion. This involves the scanning and uploading of documents through a pipeline, setting the stage for further processing.
Data preprocessing. This utilizes various techniques to prepare documents for analysis, such as format normalization, image enhancement, and optical character recognition (OCR) to convert images into machine-readable text.
Data validation. This ensures the accuracy and completeness of the data extracted from documents. AI algorithms cross-verify extracted data against predefined rules and patterns to identify and rectify errors or inconsistencies.
Data extraction. At this stage, AI identifies and extracts relevant data from the documents. Machine learning models are trained to recognize and categorize information, such as patient details, treatment codes, and billing information.
Data exportation. Extracted data are stored and presented. This step involves converting processed data into formats that are useful for further analysis or integration into other systems, providing valuable insights and supporting decision-making processes.
Completeness Checking at the Start of the Process
At the onset of care management and claims administration, ensuring the completeness of necessary documents and data is critical. AI excels in automating the verification of document sets to confirm that all required information is present and correctly formatted before further processing. These systems scan through electronic health records (EHRs), insurance claims forms, and other related documents to detect any missing or inconsistent information. By leveraging AI for completeness checks, health care providers can significantly reduce the rate of claims denials due to incomplete or incorrect submissions and streamline the authorization of necessary patient care services. This automation accelerates the authorization process and enhances its accuracy, ensuring patients receive timely and appropriate care.
Correspondence Generation at the End of the Process
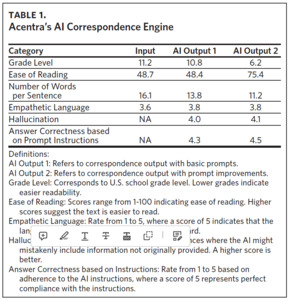
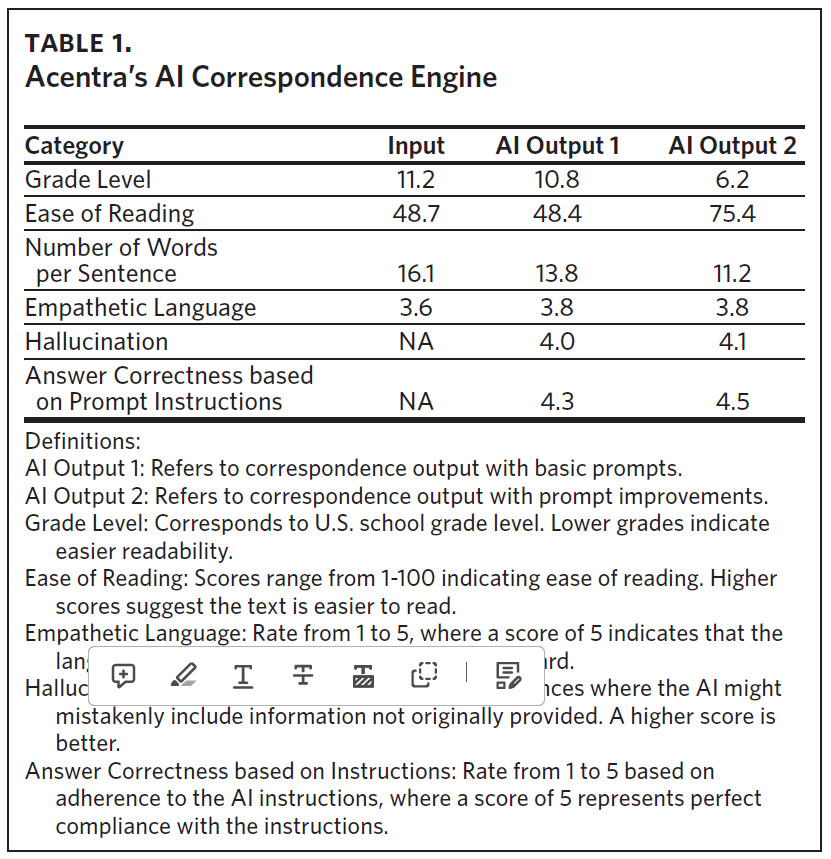
Toward the end of the care management and claims administration process, AI can significantly enhance the efficiency and quality of correspondence generation. AI-driven tools assist in drafting determination letters to beneficiaries and health care providers, ensuring that communications are not only clinically accurate but also crafted in clear, empathetic language that adheres to required readability standards. This includes adjusting the tone, style, and complexity of the message to meet specific patient or provider needs (Table 1). By automating this part of the process, AI helps to maintain consistent communication standards, reduces the time required for staff to manually compose letters, and allows for immediate feedback and necessary adjustments based on nurse interaction with the system.
To illustrate the impact of AI on just the last correspondence step, since January 1, 2024, Acentra Health’s AI correspondence engine has drafted sections of over 65,000 determination letters to providers and beneficiaries (unpublished data, Acentra Health, 2024). This has cut the average time it takes for a nurse to draft a complete document from 6 minutes and 35 seconds to just 3 minutes and 28 seconds. Additionally, the response rate from nurses using the thumbs up/down feedback system has improved, dropping from .4% thumbs down rating in January 2024 to just .03% thumbs down rating in April 2024, demonstrating a substantial enhancement in both efficiency and user satisfaction.
The improved metrics in AI Output 2 demonstrate the advancements in AI technology to produce more reader-friendly, accurate, and empathetic correspondence, adhering closely to the mandated CMS Guidelines for Effective Writing, which stipulate a Grade Level of 9 and the number of words per sentence to be fewer than 20.1 Time studies and interactive nurse feedback systems have boosted efficiency and user satisfaction, raising the quality of communication to meet rigorous CMS standards (unpublished data, Acentra Health, 2024).
Collaborative Intelligence: Enhancing Human Capabilities
The concept of collaborative intelligence refers to the use of AI to support human workers without replacing them. In health care, this means AI tools assist clinicians and administrators by providing data-driven insights that enhance decision-making processes. For example, AI can summarize and reference extensive medical records to aid in clinical validation, ensuring that health care providers operate at the top of their licenses.
Ensuring Quality and Reliability Through AI
Maintaining the quality and reliability of AI-driven processes in health care requires:
Human-in-the-Loop (HIL). Placing human judgment at the forefront is essential for validating AI outputs. This approach ensures that the health care provided aligns with professional standards and patient needs, integrating human expertise in critical decision-making processes.
Collaboration and Reinforcement Learning from Human Feedback (RLHF). This methodology combines the collaborative nature of AI applications with continuous expert feedback to enhance AI performance. Clinical experts provide insights that refine AI behavior, ensuring systems replicate the decision-making quality akin to health care professionals and adapt to clinical standards effectively.
Inter-rater Reliability. Traditionally used to evaluate consistency and agreement among clinical staff, inter-rater reliability has been incorporated into the AI review quality control process. It measures the consistency and agreement between human evaluators and AI systems in tasks such as extracting, summarizing, and documenting clinical information. This integration ensures that AI tools maintain high standards of accuracy and reliability in their operations, mirroring the meticulous validation processes applied to human staff.
Legal and Compliance Considerations
As AI becomes more integrated into health care, it is crucial to navigate the legal and ethical implications carefully. This includes adhering to evolving regulations and considering the long-term impacts of decisions made today. Concerns such as data privacy, data ownership, and the potential for AI to generate biased outcomes must be critically assessed and managed.
The regulation of AI, especially in health care, lags technology’s rapid development. It is essential to comply with existing regulations while also considering future legal landscapes. Health care administrators and AI developers must stay ahead of the curve, ensuring their AI systems are prepared to meet current and future regulatory standards as well.
Key Issues to Address in this Context
Transparency. “Right to know” themes are emerging globally, which may require organizations using AI to make the public generally aware of how they use AI in their products and services. In some cases, notice to individuals may be required if processes driven or informed by AI may have an impact on personal health outcomes.
Hallucinations in AI Output. AI-generated hallucinations, or incorrect fabrications in data output, present a significant challenge. However, advancements in AI model accuracy and the layering of models (stacking) are expected to mitigate these errors over time.
Bias in Data. Data bias is a persistent issue that can lead to skewed AI decisions. Identifying and correcting biases within training datasets is crucial for developing fair and effective AI systems.
Data Ownership and Privacy. Questions surrounding data ownership and privacy include whether health care entities own the data they use, if they have the rights to use these data for model training or tuning, whether appropriate data use agreements are in place, and how they should handle copyright issues.
Tidal Wave of Synthetic Data. With the rise of large language models (LLMs), a massive influx of synthetic data is anticipated. LLMs’ ability to interact with and modify all forms of data introduces new complexities in data management and regulation.
Navigating these issues requires a proactive approach to compliance and ethics in AI deployment. By fostering a culture of responsibility and ethical consideration, health care organizations can leverage AI’s benefits while minimizing potential harms and aligning with both current and forthcoming regulations.
Government Policy Implications
Policy frameworks at all levels must evolve to keep pace with technological advancements in AI. This includes creating guidelines that ensure safe and effective AI use while promoting innovation and protecting patient rights. For organizations like Acentra Health, which is heavily focused on delivery of Medicare and Medicaid services, adhering to current and emerging government policy frameworks is critical to ensure compliance and responsible deployment of AI technologies.
Acentra Health has established a 16-member AI council, co-chaired by our Chief Analytics Officer and Chief Legal and Compliance Officer, to spearhead internal strategies for the responsible and ethical use of AI. This council is instrumental in navigating the complex regulatory environments associated with government health care programs. It focuses on several key areas:
Governance. Establishing robust governance structures to oversee AI initiatives and ensure they align with organizational goals and regulatory requirements.
Legal and Compliance Alignment. Ensuring that AI applications adhere to all relevant laws and regulations, particularly those governing Medicare and Medicaid. This alignment is crucial for mitigating risks and enhancing compliance across all AI-driven processes.
Outcome Measurement. Developing metrics and benchmarks to evaluate the effectiveness and impact of AI technologies. This focus on measurement helps to quantify the benefits of AI applications in health care settings and ensures that they deliver tangible improvements in patient care and administrative efficiency.
Conclusion
The incorporation of AI into health care is transformative, offering significant improvements in both patient care and administrative efficiency. However, it requires a balanced approach that rigorously considers legal and ethical implications to ensure that AI deployments enhance service delivery and meet all regulatory requirements.
Acknowledgments
Disclosure of interests. All authors are employees of Acentra Health.