It is well known that pregnant people with COVID-19 are at an increased risk of severe complications for both the pregnant person and the fetus.1 Compared to non-pregnant adults, pregnant persons are more likely to require critical care admission, invasive ventilation, and/or extracorporeal membrane oxygenation and are also more likely to die.2 COVID-19 infections are also associated with increased adverse pregnancy outcomes, such as preterm birth, preeclampsia, and stillbirth.2 Despite this, in early 2021, less than 20% of pregnant individuals in the United States had received one or more doses of the COVID-19 vaccine, and by the end of the year, this increased to only just above 40% according to the United States Centers for Disease Control and Prevention (CDC).3
Barriers to receiving care, including accessing vaccinations, contribute to obstetric patients remaining unvaccinated throughout pregnancy and once postpartum. There are a variety of reasons individuals may not get vaccinated, including but not limited to language barriers, receiving misinformation regarding the vaccine, lack of regular health care/providers, and a lack of trust in health care/providers, as well as challenges with transportation and paid time off to obtain vaccinations.4–6 While vaccine accessibility is one component affecting vaccination status, another component may be vaccine hesitancy. General vaccine hesitancy within an obstetric population has been previously evaluated, with evidence showing clinician counseling as a contributing factor in consenting for vaccination.7 COVID-19 vaccination hesitancy among pregnant patients may stem from the fact that pregnant patients were excluded from the initial phase 3 clinical vaccine trials, resulting in limited data regarding the efficacy and safety of the COVID-19 vaccinations in pregnant patients.7 In June 2021, preliminary data were reported from a vaccine surveillance system of over 35,000 pregnant people, which did not show any significant increased risk of adverse outcomes such as pregnancy loss or preterm birth.8 Additionally, the American College of Obstetrics and Gynecology and the Society for Maternal-Fetal Medicine released statements recommending COVID-19 vaccinations for all pregnant patients in July 2021.9,10 Nonetheless, vaccine hesitancy still exists during pregnancy. Commonly reported reasons for not getting vaccinated during pregnancy include lack of data about safety in pregnancy and concern about potential harm to the fetus.11,12 The postpartum period presents a unique opportunity to vaccinate patients whose primary concern regarding the vaccine is its administration during pregnancy.
The objective of this chart review was to assess the vaccination status of obstetric patients prior to admission for delivery and vaccination administration once postpartum. Our hospital initiated an inpatient COVID-19 vaccination program for all units in January 2021. Recognizing the opportunity for vaccine administration in postpartum patients, we conducted a retrospective chart review to evaluate vaccination status and administration among all postpartum patients during six months in 2021.
Methods
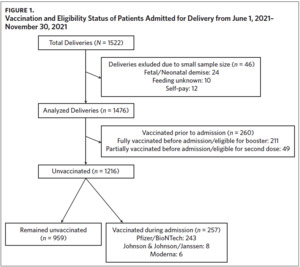
We analyzed data from 1,476 of the 1,522 patients who were admitted for delivery at WakeMed Hospital in Raleigh, North Carolina, during a six-month period (June 1, 2021–November 30, 2021) (Figure 1). The 46 patients not included in this analysis were those who had fetal or neonatal demise, an unknown mode of feeding, or those who were self-pay; due to small numbers in each group (fetal or neonatal demise, unknown mode of feeding, or those who were selfpay), analysis could not be performed and thus these data were excluded in the final analysis. All patients admitted to WakeMed Hospital, including patients who were excluded in the analysis, were counseled and offered vaccination. This chart review was granted an exemption by the Institutional Review Board at WakeMed Health and Hospitals.
Vaccination status prior to admission was determined by chart review in the electronic medical record and through searching in the state immunization registry. Individuals considered “fully vaccinated” prior to admission were patients who completed at least two doses of the two-dose series for Moderna or Pfizer-BioNTech (Pfizer) or completed one dose of Johnson & Johnson/Janssen (J&J).13 Fully vaccinated individuals included those who may have also received a booster dose. Partially vaccinated individuals prior to admission were patients who completed one dose of the two-dose series for Moderna or Pfizer. Patients were eligible for vaccination if they had not received the first dose of the COVID-19 vaccine, were due for the second dose or booster, did not have an active case of COVID-19, and/or had not received monoclonal antibodies in the prior 90 days. Eligible patients were offered vaccination and counseled by their provider(s) during their hospitalization; there was also documentation of individuals who chose to decline vaccination. At the time of this intervention, WakeMed Hospital offered vaccination to all hospitalized patients; however, COVID-19 vaccination was not in routine postpartum order sets for individuals without documented vaccination. Upon hospital admission, all patients were tested for COVID-19. Individuals who tested positive were not offered vaccination during their hospitalization. COVID-19 vaccines offered to patients while inpatient included Moderna, Pfizer, and J&J. Of note, patients who were eligible for the second dose of the COVID-19 vaccine (n = 49) or booster (n = 211) were also offered the vaccine but were not included in data analysis for those who received vaccination during hospitalization once postpartum (n = 260).
For statistical analysis, ANOVA was used to analyze our continuous variables: maternal age and gestational age. Chi-squared was used to analyze the statistical significance between groups of different vaccination statuses within our categorical variables, which included parity, race/ethnicity, insurance type, mode of delivery, and mode of feeding at the time of discharge. Of note, “race” and “ethnicity” were not separated on the hospital intake demographic form; more information on demographics was not provided (or available) at the time of data collection. P-values less than .05 were considered statistically significant.
Our primary outcome, vaccination status (vaccinated prior to admission, vaccination administration during hospitalization, and unvaccinated at discharge), was analyzed via multinomial logistic regression, with the reference group comprising those who remained unvaccinated at the time of discharge. Our covariates included age in years, gestational age in months, parity (nulliparous and multiparous), race/ethnicity (Asian, Black/African American, Hispanic/Latino, Other/Unknown, White/Caucasian), mode of delivery (vaginal and cesarean), mode of feeding at the time of discharge (breastfeeding/pumping and formula), and type of insurance (private and public/government). The results are reported as relative risk reductions (RRR).14
RRR is another way of describing risk ratio (RR); it is calculated as 1 minus the relative risk.15 RR compares the risk of an event (e.g., vaccination before admission) occurring within a group (e.g., multiparous) compared to the reference group (e.g., nulliparous).15 RRR expresses RR as a percentage of reduction. Relative risk reduction was the preferred method for data analysis, as it presented results with less bias. While multinomial logistic regression analysis could have been done with these data in order to adjust for confounding variables, previous research has shown that odds ratios in logistic regression often overestimate the odds of an outcome occurring.16 Additionally, logistic regression is commonly used when the incidence is rare (less than 10%), which would be an inappropriate method for our analysis as our outcomes were common, e.g., vaccination status.17 Lastly, logistic regression cannot account for variable outcomes if there is a natural order between those outcomes. For example, in our chart review, vaccination status is divided into three outcomes: vaccination prior to admission, during hospitalization, and at discharge. Because vaccination status may change during hospitalization (e.g., the patient was offered the vaccine and accepted), logistic regression would not be able to determine how this vaccination status would change vaccination statistics at discharge. Thus, given this example, multinomial logistic regression would be inappropriate, which further supports our use of relative risk reduction.
Results
From June 1, 2021, to November 30, 2021, there were 1,522 patients admitted for delivery, of which 1,476 were analyzed (Figure 1). Of these patients, 260 (17.6%) patients were either fully vaccinated (81.2%; n = 211) or partially vaccinated (18.8%; n = 49) prior to admission, which meant 1,216 (82.4%) patients were unvaccinated at the time of admission to the hospital. Of the unvaccinated postpartum patients, 257 (21.1%) received a vaccine dose, which included vaccines from Johnson & Johnson/Janssen (3.1%; n = 8), Moderna (2.3%; n = 6), and Pfizer/BioTech (94.6%; n = 243).
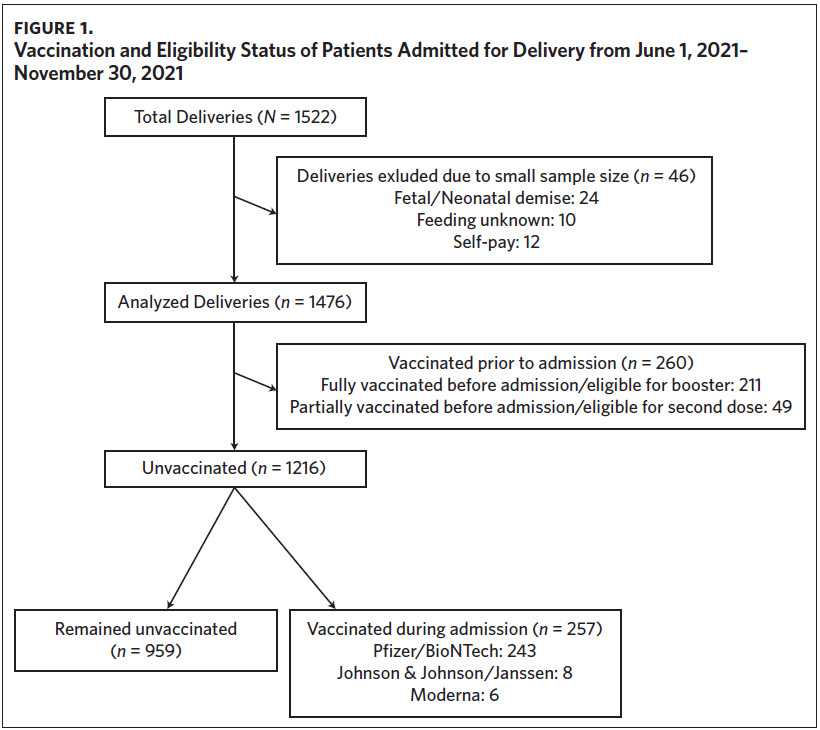
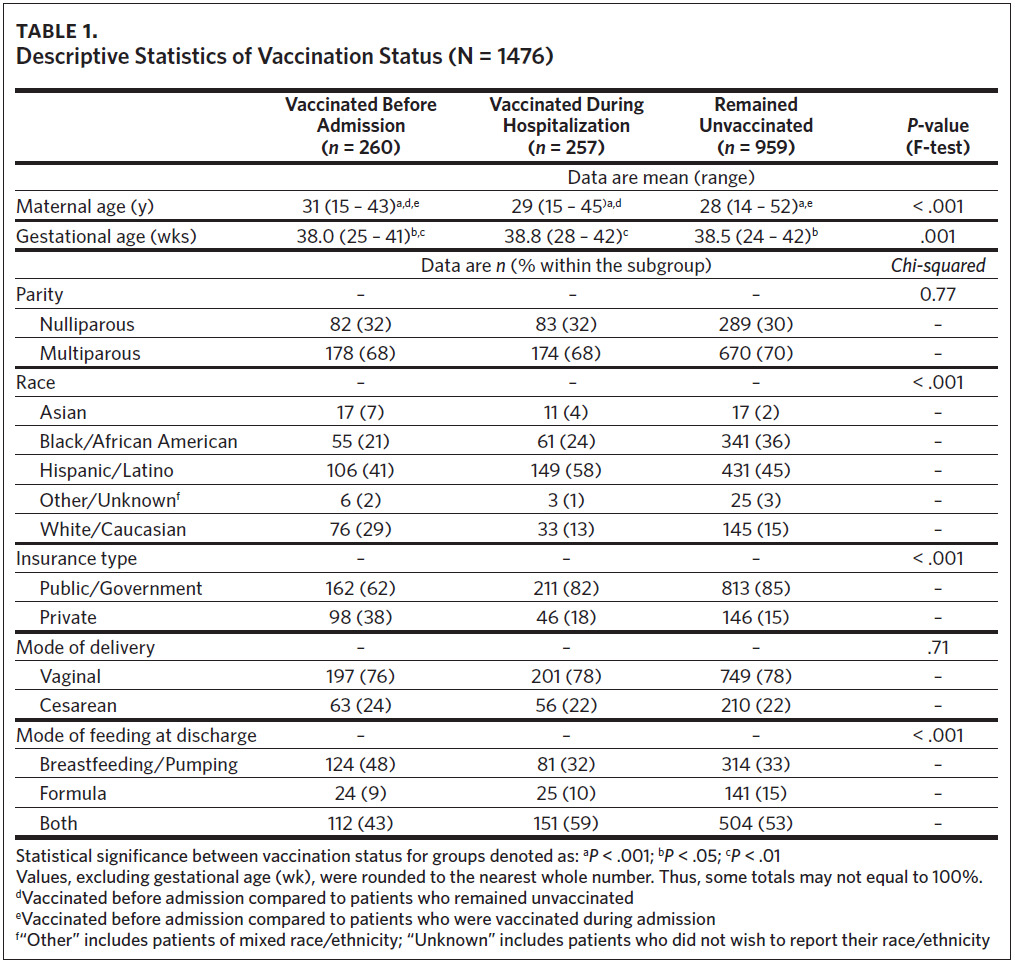
Table 1 shows descriptive statistics of patients vaccinated before admission, those vaccinated during hospitalization (received the vaccination once postpartum), and those who remained unvaccinated at the time of discharge. The majority of patients, regardless of vaccination status, were multiparous and Hispanic/Latino, received public or government insurance, and had a vaginal delivery. Patients who were vaccinated prior to admission were more likely to exclusively breastfeed or pump as a mode of feeding, while those who were vaccinated during hospitalization or remained unvaccinated at discharge were more likely to both breastfeed/pump and use formula.
Table 2 shows the result of a multinomial logistic regression of patients vaccinated prior to and during hospitalization compared to those who remained unvaccinated (the reference group). Among our population, the odds of being vaccinated increased with increasing age. The RRR was 1.03 for vaccination in pregnancy and 1.08 for vaccination postpartum, representing 3% and 8% increased odds of vaccination for each additional year of maternal age. Black patients were less likely to receive a COVID-19 vaccination prior to admission (RRR = 0.44) than White patients. Asian patients and Latina/Hispanic patients were more likely than White patients to receive a vaccine during their hospital stay (RRR = 2.79 and 1.73). Further, the odds of being vaccinated prior to admission versus remaining unvaccinated were 2.51 times higher for those with private insurance compared to those with public/government insurance.
Discussion
With increasing age, the odds of receiving the vaccine increased. Regarding race/ethnicity, Asian and Hispanic/Latino patients were more likely to get vaccinated during hospitalization compared to White patients. Black patients were less likely to get vaccinated during hospitalization compared to White patients. Lastly, those who were vaccinated were more likely than unvaccinated individuals to have private insurance compared to those with public/government insurance.
The findings of this chart review are similar to those of a smaller study that evaluated COVID-19 vaccine administration in a postpartum population with regard to overall vaccine rates both prior to and during hospitalization for delivery. Perez and colleagues found that 22.8% of their total sample (n = 329) had been vaccinated prior to admission.18 Of their unvaccinated patients, 23.5% received vaccination, with 76.5% declining vaccination during hospitalization.13 The current chart review found nearly identical rates of pregnancy and postpartum vaccination in a much larger sample of women. The numbers of people who received vaccination (21.1%) and declined vaccination during hospitalization (78.9%) persisted among our patient sample with a sample size that was nearly five times larger (n = 1476).
Although vaccine acceptance and administration overall has continued to improve, throughout 2021 the average vaccination rate for pregnant individuals in the United States peaked at just above 40%, which is higher than the vaccination rate of our cohort during pregnancy (17.6%).3 Pregnant and postpartum populations continue to be an under-researched population with respect to COVID-19 vaccination; state data, specifically in North Carolina, on vaccination rates in these populations were not available.
In our population, we had significantly higher proportions of Black/African American (31.0% versus 14.4%) and Hispanic/Latino patients (46.5% versus 25.1%) compared to the national averages of pregnant individuals of these race/ethnicities.19 These differences in proportions of racial/ethnic groups among our cohort may explain the lower rates of COVID-19 vaccination during pregnancy compared with the national rate, as racial disparities in both vaccine access and acceptance have been documented.20 Data have shown rates of vaccination among White individuals compared to Black and Hispanic/Latino individuals being two to four times higher.21,22 This difference in vaccination rates has been attributed to historical mistrust and mistreatment among these populations in health care, as well as concerns regarding vaccine side effects and a lack of sufficient research.23,24
Vaccine hesitancy or health care mistrust may not be the only reasons that individuals do not get vaccinated. Our chart review found that there was a higher proportion of Hispanic/Latino patients who received vaccination during hospitalization compared to their White/Caucasian counterparts. While vaccination rates have generally been reported to be lower among Hispanic/Latino populations, there are data that show higher rates of vaccine endorsement or intent among this population.21 Other barriers to accessing care and therefore vaccinations, such as lack of staffing for vaccine administration, travel distances to access care, and vaccine availability in a geographic location, may also negatively impact vaccination rates even if there was intent or desire to become vaccinated.25,26 The inpatient setting may have provided a unique opportunity for access among patients who were interested in being vaccinated and perhaps had not remained unvaccinated only due to pregnancy.
The strengths of this chart review included a large sample size with a diverse population. Because all postpartum individuals were counseled, which was not a standardized practice throughout WakeMed Hospital, this strengthened our findings as we were able to better characterize our population. Additionally, counseling promoted easy accessibility to vaccines and an opportunity to address fears and/or hesitancy in becoming vaccinated. Vaccination was also offered to spouses and family members of postpartum individuals to further promote primary prevention of COVID-19 infections. Through this approach, we were able to provide vaccinations to populations that may not otherwise get vaccinated (e.g., rural communities and high-risk populations).
There were several limitations to our chart review. At the time of our intervention, vaccination counseling and administration had not been added to standardized order sets, thus providers were responsible for counseling and offering the vaccine. Because there was no standardized way of counseling, variations in counseling may have impacted patient acceptance. While this intervention focuses on the vaccination status pre- and post-hospitalization, identifying variations in counseling techniques may be beneficial in future studies. After this intervention was completed, a COVID-19 vaccination fact sheet, written in English and Spanish, was developed and provided to all hospitalized patients at WakeMed Hospital.
One limitation is that we did not collect data on COVID-19 infection status of the patient at the time of admission (e.g., if they had contracted the COVID-19 virus and had recovered by the time of admission). Additionally, there are no qualitative data about reasons for not getting vaccinated prior to admission or declining vaccination during hospitalization. Given that reasons for declining or deferring vaccination are complex, more information about patients’ access to care, beliefs, and reasoning may help target future efforts at education, counseling, and administration. Given our higher proportions of Black/African American and Hispanic/Latino patients compared to national averages, selection bias could be of concern in our data analysis. However, WakeMed Hospital is a large urban hospital that provides care to all locals and those who are referred. All individuals who were admitted for delivery at WakeMed were reviewed for this intervention, thus selection bias is not considered a limitation. Given the difference in demographics between our population and national averages, the generalizability of our intervention as a representation of state or national populations could be considered a limitation.
Conclusion
COVID-19 vaccination status differed by maternal age, race/ethnicity, and insurance status, but not by gestational age, parity, delivery or feeding methods. Pregnant individuals continue to have lower rates of vaccine acceptance and administration, despite evidence revealing higher rates of complications during pregnancy and higher rates of the disease itself among pregnant individuals. The postpartum period is a unique opportunity to improve vaccination rates among this population; however, our results show that among a diverse population of postpartum patients, differences in vaccination status during pregnancy and after delivery persist between individuals of different races/ethnicities, ages, and insurance statuses. Further research is needed to better understand barriers to access as well as reasons for declining COVID-19 vaccination, particularly among groups identified as having lower rates of vaccination uptake.
Acknowledgments
The authors thank Amanda Edwards, MMS, PA, for her help in leading the vaccine administration program and obtaining the administration data. Ms. Edwards is employed at the WakeMed-Raleigh Campus and has no disclosures or funding statement. We also thank The Howard W. Odum Institute for Research in Social Science at UNC-Chapel Hill for help with data analysis. The Odum Institute has no disclosures or funding statements.
Declaration of interests
The authors declare there is no conflict of interest.
Author contributions
Lisa P. Michelson, MA, MPhys participated in research design, in the writing of the paper, in the performance of the research, and in data analysis, managed the progression of this manuscript, and had final approval of the final version to be published. A. Jenna Beckham, MD, MSPH participated in research design, in the writing of the paper, in the performance of the research, and in data analysis, and had final approval of the final version to be published. A.J.B. is a Medical Expert/Health Advisor for Flo Health, Inc.
Funding
None.