Introduction
Health outcomes are largely influenced by a complex interplay of various non-medical factors, often described as social drivers of health. The North Carolina Department of Health and Human Services estimates that up to 80% of a person’s health is determined by social and environmental factors, rather than high-quality medical or dental care alone.1 Social drivers of health are grouped into the following five domains: economic stability, education access and quality, health care access and quality, neighborhood and built environment, and social and community context.2 When unpacked further, these domains explore how life experiences such as unemployment, poverty, social discrimination, attending an underfunded school, or living in a neighborhood with high rates of violence can have a direct impact on an individual’s health outcomes. However, one cross-cutting aspect often underemphasized in descriptions and definitions of social drivers of health is the impact of culture. Cultural factors intersect with each of these five domains and have been shown to significantly impact individuals’ health beliefs, behaviors, help-seeking patterns, and health utilization.3 This perspective piece explores why cultural influences are especially notable in oral health care, and why the presence of culturally attuned care should be viewed as a critical social driver of oral health. Additionally, specific recommendations are made on how to increase culturally attuned care in the oral health field to improve patient health outcomes.
Cultural Influences on Health
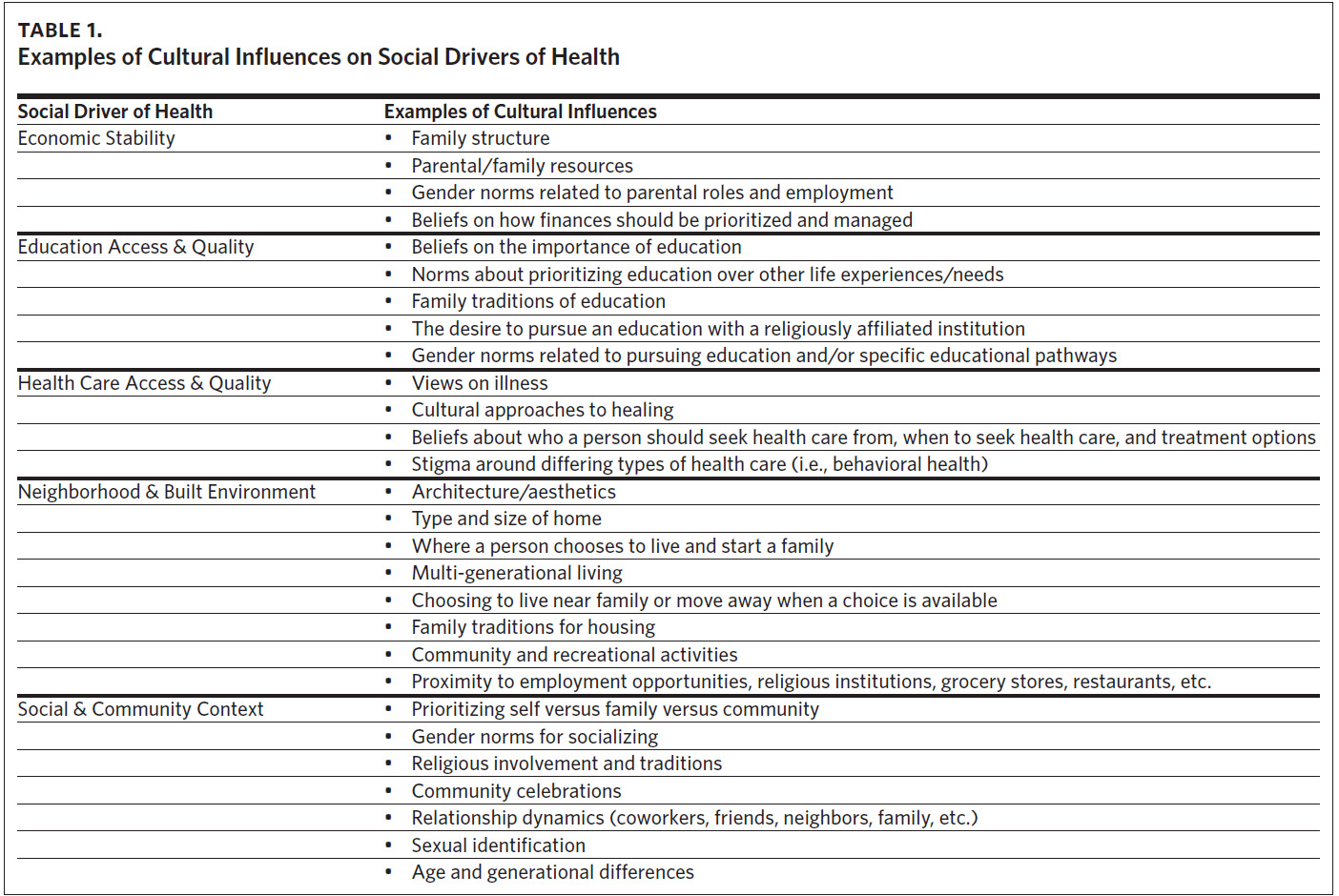
Culture is defined by social worker and researcher Cindy Garthwait as “beliefs, ideology, worldview, and values common to a group of people and which guide their individual and social behavior… specifically, it is the product of the values, ideas, perceptions, and meanings which have evolved over time”.4 Culture has a direct impact on the health of individuals as it shapes health beliefs, practices, and behaviors. In oral health, we see culture influence how people engage in their dental visits, manage their home hygiene practices, perceive treatment recommendations, and adhere to treatment plans. Culture can also influence social drivers of health, which can in turn have a strong impact on how a patient views and engages with their overall health and subsequently their oral health. Table 1 provides a few examples of how social drivers can be influenced by culture.
By utilizing a culturally attuned approach to patient care, oral health providers can integrate cultural elements of a patient’s life into their understanding of who a patient is as a person, improving the ability to address not only the medical needs of that patient but the social drivers of their health as well.
Culturally Attuned Care in Oral Health
Culturally attuned care is a person-centered approach to patient care that recognizes the importance of cultural factors and strives to provide care that is respectful of and responsive to patients’ unique cultural needs. This is an alternative to the traditional approach to cultural competency, which implies there is an endpoint or fixed place for cultural knowledge where one can say they have arrived. Alternatively, cultural attunement describes an individualized approach to patient care that recognizes humans to be complex and layered rather than a two-dimensional list of cultural factors that can be found in a textbook. Understanding why individuals hold certain beliefs about their health, or why they make certain decisions, goes beyond having a basic understanding of various cultures. Being a culturally attuned health care provider means getting to know your patients beyond their body, their teeth, and beyond what you think they may feel or believe about their health. This approach does not mean a provider has to have impeccable communication skills, advanced screening protocols, or a keen understanding of global cultures—it simply requires a desire to genuinely get to know your patients and their health care goals at an intimate level. This care also requires humility and the ability to respect a patient’s opinions and beliefs when they are different than your own. While individual provider self-reflection is critical, systems hold equal if not greater responsibility for identifying and addressing oral health inequities.
Recommendations
Ingraining culturally attuned care into standard oral health care provision will require action at various levels, ranging from dental student recruitment and pre-doctoral dental education accreditation standards to widely adopted clinical practices.
Pre-doctoral Dental Education Accreditation Standards
Statistics show that the oral health workforce does not accurately reflect the racial demographics of the US population, and many of those who are currently practicing dentistry lack crucial skills needed to provide tailored care to diverse populations.5 The Commission on Dental Accreditation (CODA) attempts to acknowledge the importance of better equipping future dentists with the skills needed to serve a diverse patient population by including “basic principles of culturally competent health care” into standard 2–17.6 However, the term “culturally competent” is an outdated and inaccurate representation of the skillset needed to serve a diverse patient population, as competence indicates an endpoint in knowledge. A starting point for the necessary paradigm shift to culturally attuned care as a standard of care in oral health is to utilize more accurate language for this critical skillset. This shift in CODA accreditation standards influences the relevant clinical and pre-clinical content in pre-doctoral education nationally.
Dental Student Recruitment
Though updating accreditation standards is an important step in preparing future dentists to serve a diverse patient population, the dental education system also holds the responsibility of graduating a diverse dental workforce that represents the patients it serves. According to the US Health Policy Institute, in 2020, 70.2% of dentists were White, 18% were Asian, 5.9% were Hispanic, and 3.8% were Black.7 However, this workforce does not represent the US population, as statistics show racial demographics to be 70% White, 5.6% Asian, 18.4% Hispanic, and 12.4% Black.8.
Within the next 25 years, people of color are expected to comprise most of the US population, yet racial inequality and underrepresentation in the oral health workforce will likely persist.9 Policy decisions about oral health often center the interests of White and Asian providers, but not the providers who identify with communities at the highest risk of oral health complications—Black, Hispanic, and American Indian/Alaska Native.5 Until we have a dental workforce that represents the patients served, culturally attuned care will continue to be an exception to the standard of oral health care, and oral health disparities will persist. Therefore, it is imperative that pre-doctoral dental education programs pursue fresh approaches to recruiting a more diverse student group including but not limited to: partnerships with middle and high schools to introduce dentistry at an early age; immersive exposure experiences and pipeline entry programs for Historically Black Colleges and Universities (HBCUs); mentor opportunities for enrolled dental students from minoritized groups to partner with interested students from similar backgrounds; and strong diversity, equity, inclusion, and belonging programs at all pre-doctoral dental schools to address systemic and individualized supports for students from diverse backgrounds to promote retention and success.10
Clinical Practice
Regardless of setting or specialization, there are multiple approaches to implementing culturally attuned care practices into oral health care delivery, from practice management to standards of clinical care. Practice management approaches start with increasing the accessibility of services for a diverse patient population through offering flexible payment plans and sliding-scale fees and being in-network with a wide range of dental insurance plans. Recognizing and addressing cultural barriers that traditionally exist in oral health environments, such as language differences and mistrust of the health care system, can improve access to care. Providing adequate interpretation services and culturally relevant patient education materials in various languages can make health care more accessible. Visual aids can also enhance comprehension and understanding. Marketing strategies should be rooted in community needs and desires and include the engagement of community organizations, local leaders, schools, and faith centers. Additionally, oral health providers should take an active part in their communities beyond their practices’ dental chairs by advocating for local, state, and federal policy changes that promote positive outcomes for the most underserved and marginalized communities. By being present within the community, oral health providers can increase accessibility to their practice while serving as resources and advocates in their communities and promoting trust and relationship-building with the people who live there.
To advance direct patient care, a targeted approach should be taken to implement strategies and patient care workflows that enhance patient-provider communication, build trust with the oral health team, and empower patients to articulate their health perspectives and care goals. Doing so enables oral health providers to provide accurate diagnoses and treatment that coincide with patients’ personal health beliefs and cultural traditions. This approach also ensures that patients thoroughly understand their oral health conditions and feel confident in managing them. Beyond informal rapport building with patients, there are a few structured options for learning more about a patient’s cultural health factors. Incorporating social history questions into comprehensive new patient exams can provide extensive insight into a patient’s life beyond the physical health of their body and mouth. These questions should primarily address social drivers of health and health beliefs, and may be open- or closed-ended, depending on the provider’s preference. Many publicly accessible screening tools for social history and health beliefs exist that are commonly used in medical settings and are either ready for immediate implementation into the oral health setting or can be easily adaptable. Additionally, many electronic health records (EHRs) feature social history questions or screening tools built into their health history sections, enabling patients to complete these questions prior to appointments, at check-in, or during conversation with an oral health team member while sitting in the dental chair. Utilizing any of these approaches leads to a better understanding of patients’ needs, goals, and preferences, ultimately resulting in improved health outcomes.
Conclusion
Integrating culturally attuned care as the standard practice in oral health care is essential to effectively address oral health disparities. By recognizing and respecting patients’ cultural backgrounds and their impact on patients’ health behaviors and goals, health care providers can offer more accurate and efficient treatments while patients become more engaged in their health care journey. Culturally attuned care enhances the critical social drivers of health such as economic stability, education, social and community support, access to health care, and the built environment. Achieving this new standard of care requires systemic changes, including updates to pre-doctoral dental education accreditation standards and proactive recruitment of a diverse dental workforce. Additionally, clinical practices must adopt strategies that improve accessibility, patient-provider communication, and community engagement. Only through these concerted efforts can we hope to reduce oral health disparities and promote equitable health care for all.
Acknowledgments
All authors confirm that there are no conflicts of interest.