Gregory Chadwick, DDS, MS, has served as Dean of the East Carolina University (ECU) School of Dental Medicine since 2012, just a year after the school admitted its first class. Chadwick led the effort to establish the school in his previous capacity as Associate Vice Chancellor for Oral Health at ECU, a role he took on after nearly 30 years of practicing dentistry in Charlotte.
Guest editors Crystal Adams, MA, CDA, RDH, Associate Director of the North Carolina Oral Health Collaborative, and Steve Cline, DDS, MPH, Vice President of the Foundation for Health Leadership & Innovation, spoke with Chadwick about the ECU School of Dental Medicine’s educational model and the role and impact of Community Service Learning Centers, particularly in rural areas.
“We have 508 graduates so far, and they come from 87 counties, and almost 90% of our graduates are practicing in North Carolina,” said Chadwick.
This interview has been condensed and edited for clarity.
Crystal Adams, NCOHC: Can you talk about how your model at ECU is different from other educational models in North Carolina or other states?
Greg Chadwick: The things that are important to us are the same things that are important to all dental schools, but our mission is a little unique in that we were funded to help improve the oral health of the people of North Carolina, and our focus has been on rural North Carolina. Every dental school has the mission to improve the oral health of whatever that region may be, and to educate the next generation of dentists. Ours, in addition to that, is to provide a significant amount of care to rural populations.
As a newer state-funded school, we accept only North Carolina residents. Why? Because we feel like, especially in rural areas, the folks who are from those rural areas are more likely to return home to practice.
Adams: Can you go into a little bit of detail about the Community Service Learning Centers?
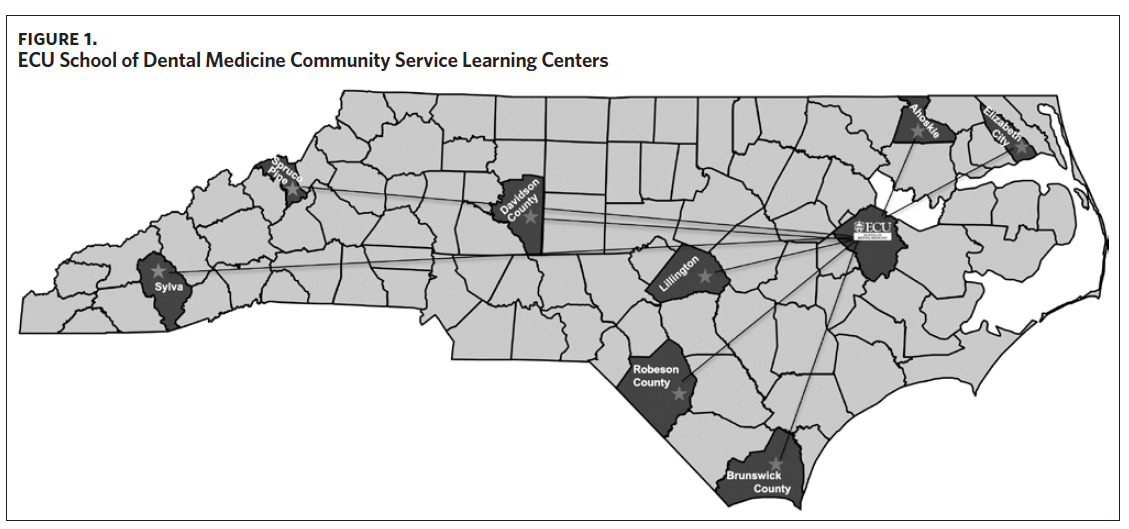
Chadwick: The Community Service Learning Centers (CSLCs) are really one of the unique features of our model. We have eight CSLCs located in rural areas across the state, all the way from Sylva in the far west to Elizabeth City in the northeast, to Brunswick County in the southeast (Figure 1). Our goal is to provide a dental home in areas where there aren’t enough dentists to take care of the population. CSLCs are owned and operated by the dental school, and each have 16 operatories, so you can look at them as large dental clinics or as small dental schools, but they’re each independently operated. Each has full-time faculty, a full staff, an office manager, and six learners. Four learners are senior dental students who are on nine-week rotations and two are residents in a one-year Advanced Education in General Dentistry residency program. Each dental student rotates to three different CSLCs during their senior year. The CSLCs provide a full range of general dental services in these areas—they’re not just emergency clinics; they don’t just do extractions. About 30% of our patients at the CSLCs are Medicaid patients, but we also see patients who have insurance as well as private pay fee-for-service patients. Our model focuses on developing leaders who, when they graduate, are going to have an impact on North Carolina, especially rural areas of North Carolina.
Adams: I love this model, and you know I’m from a rural community. How have the ECU Community Service Learning Centers contributed to the education of the students and also to the care needs in the communities where they are located?
Chadwick: These practices are real dental practices where students see patients all day, as opposed to in a dental school where they may have a morning clinic and an afternoon clinic and they may see one or two patients during each clinic period. When they’re seeing patients in the service learning centers, they’re under the supervision of our faculty living in those communities, and they’re working with dental assistants and hygienists out there as well, just like they would in a private practice or a corporate practice type situation.
When you look at the ECU School of Dental Medicine overall, about 60% of our patients are seen in the CSLCs, and since we opened our first CSLC in 2012 we’ve provided care to over 105,000 individual patients across the complete network (internal data).
To be successful in rural areas we must be part of primary care, which means that we’re helping to change the conversation so that the public realizes that oral health is an integral part of overall health. Each of the CSLCs has affiliations with primary care providers, be that an FQHC [federally qualified health center], a public health department, or a hospital in the area. That’s an important part of who we are and who we want our graduates to be. So, when the students go to the CSLCs, they are living in those communities and experiencing life and interacting with the residents in those communities, and hopefully seeing opportunities for providing care in rural communities.
Adams: Can you describe what you see as the most challenging needs affecting oral health care in North Carolina? And how has training dental students in the CSLCs impacted the communities?
Chadwick: We have some counties still that don’t have a dentist and don’t have a physician either, and the oral health needs are great. There is a need to be able to provide a dental home for individuals in rural areas, especially in counties that don’t have any dentists. When we look at the counties that house our eight CSLCs, there are about 800,000 to 900,000 people who have access to our clinics. If you consider the counties adjacent to our clinics where people won’t have to drive over more than one county line to get to an ECU facility, then almost 48% of the state’s population has access to one of our facilities. We are meeting some of the demand with our CSLCs.
One of the challenges is helping people to see the importance of good oral health and that dental disease can be prevented. Another significant need across the state is the rapidly growing population of patients with special health care needs, and many of those are not getting the care that they need. This is very prevalent across the state, and it’s certainly more prevalent and exaggerated in the rural areas. Our school is in the process of planning a program to give our students more experience in this area while providing significantly more oral health care for patients with special health care needs.
Adams: How is ECU currently preparing students for special care dentistry?
Chadwick: We are focusing on the I/DD [intellectual and developmental disabilities] population, but we also have a number of wounded warriors, Veterans with disabilities in our state, as well as frail elderly patients and medically complex patients.
We understand that between 15% and 20% of the population has special health care needs and that about 60% of the special health care needs population or more could receive care in a general dental office if the practitioner had the necessary experience and training (internal data), and they wanted to incorporate this population into their practice. So, the opportunity is certainly there, and it’s an area of emphasis.
All of our dental students get some experience providing care for patients with special health care needs, and students with a particular interest in providing care for these patients have the opportunity to get enhanced experiences. With the current need in the state outpacing the care that’s available to this growing population, there really is an opportunity for us to do more.
We formed a group of about 25 individuals from leadership within the state, private practitioners, faculty, and educators involved with providing care for special health care needs populations who have established or directed programs within dental schools across the country. We’ve begun the conversation and planning process for an educational program, which would include research and scholarship, to give our students more experience in this area while providing more care to patients with special health care needs.
Steve Cline, FHLI: Where do you see dental education moving in the future?
Greg Chadwick: Dental education plays an important part in our profession and its future is bright. The mission areas of educating the next generation of dentists, providing care (service), and research are all very important. We need to emphasize the important role that research in dental schools plays in guiding how we teach and assess student competence and establish the evidence base for clinical practice as well the profession.
I may be a little biased, but I think we’re doing a pretty good job in all of these areas. And I suspect when you look at our model with our CSLCs, I think we’ll see more schools moving in the direction of this model if they’re able to.