Introduction
A perinatal health care workforce that is robust, well-trained, responsive, and appropriately distributed is vital to the health and welfare of our communities. This workforce encompasses a range of personnel including the physicians and advanced practice professionals (APPs) who provide maternity care to people of reproductive age and their families. Typically, this includes obstetricians (OB/ GYNs) and family medicine doctors (FMs), certified nurse midwives (CNMs), and women’s health and family nurse practitioners (NPs), although NPs do not perform deliveries and only OB/GYNs and fellowship-trained FMs perform cesarean deliveries.
The Women’s Health Care Workforce
The total supply of these professionals across the United States is under duress and forecast to increasingly fall short of demand, especially in our rural communities. Shortages will result from an anticipated increase in demand coupled with projected attrition from expected retirements and work hour reductions that will well exceed the number of new doctors entering the workforce.1,2 Reduction in work hours, as well as some number of resignations, are also expected among physicians and APPs due to high levels of “burnout”,3–5 and life and career re-evaluation taking place as part of the “Great Reprioritization” following the COVID-19 pandemic.6
The decline in physician density is notable. According to the US Department of Health and Human Services Health Resources and Services Administration (HRSA) workforce reports, in 2018 there were ~50,850 full-time equivalent (FTE) OB/GYNs in the country; by 2020, only 40,180 remained.1,2 By 2030, the estimated number falls to 30,490, a 7% decline in a workforce that will fail to meet an estimated 4% growth in demand; the 2030 projected FTE of OB/GYNs will be able to meet only 90% of projected demand.1 According to Vetter and colleagues , estimated shortages of OB/GYNs will continue to increase beyond 2030, due in part to the stagnation of OB/GYN residency program positions funded by the Centers for Medicare and Medicaid Services (CMS), which currently provide 2.5 graduates per 100,000 citizens.7 The projected OB/GYN shortages rise to 24% by 2040 and 31% by 2050.7
HRSA likewise projects that the relatively small FTE of FMs who provide maternity care will also contract. By 2030, the projected shortfall will reach 17,660 doctors; practicing FMs will be able to meet only 87% of demand.1 While approximately half of graduating FM residents intend to provide prenatal care, and 1 in 4 intend to provide full-scope obstetrics,8 half report being unable to obtain employment supportive of these intentions.9
Conversely, HRSA estimates an oversupply of CNMs and women’s health NPs by 2030.1,2 NPs remain a small but important component of the workforce providing prenatal care in community health centers near maternity care deserts.10 However, HRSA projects that APPs likewise will not find employment opportunities, and thus cannot contribute to reducing shortages of women’s health care providers.1
Women’s health care workforce shortages are variable across areas of population density and US regions. Metropolitan areas enjoy a more adequate supply while many rural counties remain maternity care deserts.1,2,10–12 Currently, over 4 million women of reproductive age live in maternity care deserts. HRSA projects that by 2030, OB/GYNS will meet 95% of demand in metropolitan areas but only 51% in nonmetropolitan areas.2 These shortages will be further exacerbated by an estimated reduction in FMs providing maternity care in nonmetropolitan areas (-6%).1
Shortages in rural areas are driven, in part, by closures of rural hospitals entirely, or partial closures via selective elimination of labor and delivery services.13 Regionally, the South has experienced the highest rate of rural hospital closures over the past three decades. Despite federal financial incentive programs, hospital closures continue to sweep across rural counties and now are seen increasingly among the nonmetropolitan counties adjacent to metropolitan areas.14 As compared to the Northeast, which has the highest current and 2030 projected physician density of the four US regions,1,12 the South fares worse. Although the South had the smallest regional deficit of physicians in 2018, it is expected to have the second-largest deficit by 2030. Specifically, the OB/GYN deficit is projected to increase from -110 FTE to -2270 FTE.1
North Carolina fares somewhat better among Southern states. HRSA reported a 2018 statewide supply of OB/GYNS equivalent to the demand. However, by 2030, North Carolina OB/GYNs will have capacity to meet only 92.8% of demand. Nevertheless, this exceeds projections for the South as a whole, at 88.7%, and the US (+DC), at 90.2%, and it places North Carolina at 19th in the nation.1
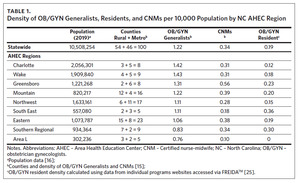
The Sheps Center for Health Services Research’s Health Workforce NC interactive report details physician density: the rate of licensed, active physicians (excluding GME residents, who may be licensed but not eligible for independent practice in a specialty after one year; as of Oct 2021) per 10,000 people (using 2019 census data) across the nine North Carolina Area Health Education Center (AHEC) regions (Figure 1).15,16 In 2021, three of the major metropolitan AHEC regions had a density of OB/GYN generalists that exceeded the state level. Two major metropolitan areas and the Mountain area (MAHEC) exceeded the state density level for CNMs (Table 1). The more rural regions of North Carolina have shortages of both types of providers.
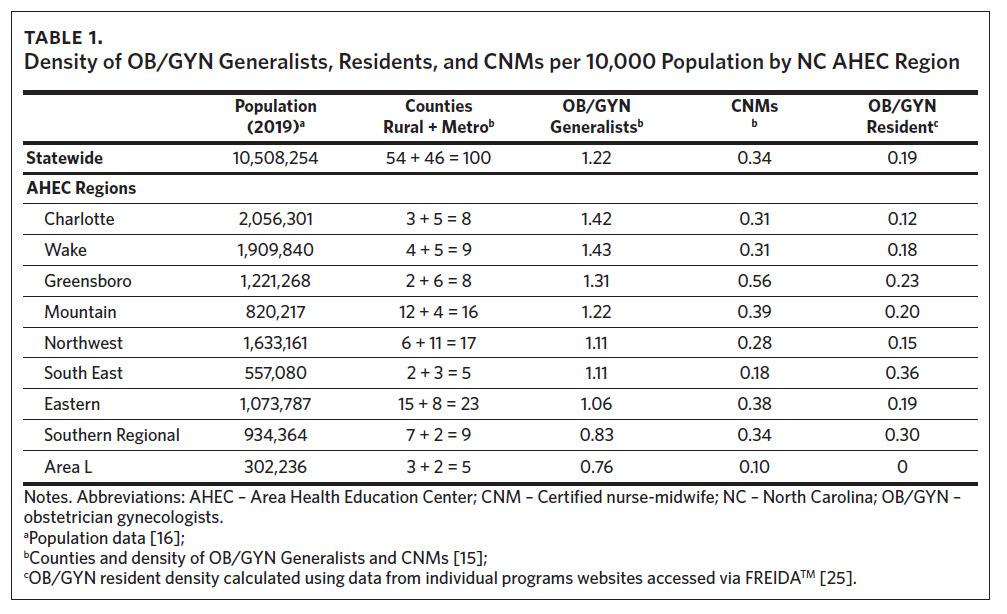
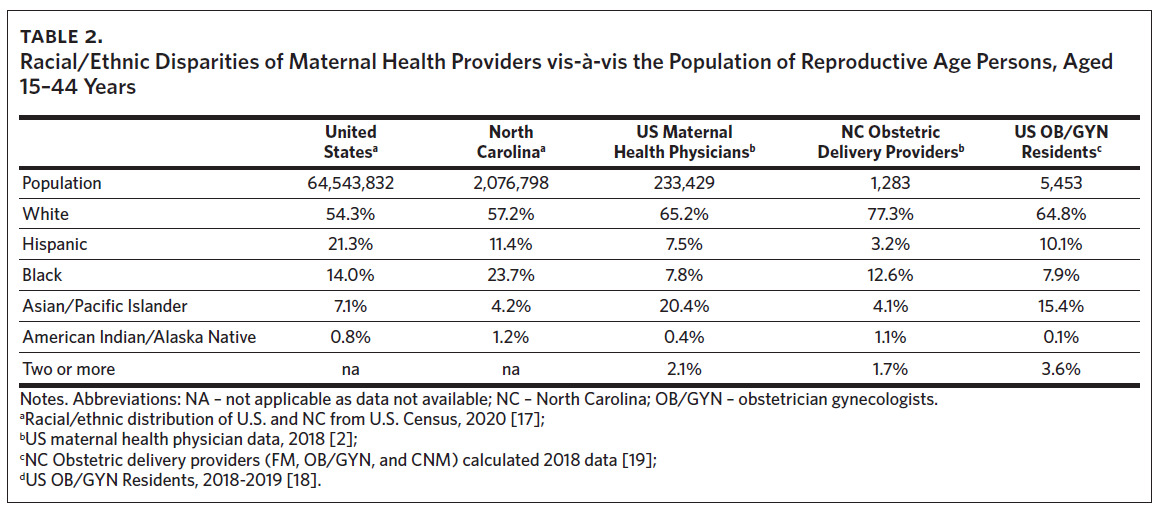
Another important consideration is the lack of racial and ethnic representation within the women’s health care workforce (Table 2).2,12,18–20 The workforce is substantially underrepresented by providers of races/ethnicities other than White or Asian/Pacific Islander.2,18 Physicians from minority backgrounds are more likely to practice in underserved areas with vulnerable populations.12 Physician-patient racial/ethnic concordance has been shown to significantly improve communication, health care utilization, and outcomes.21,22
Strategies for Meeting the Needs of All Our Communities
There are many strategies, some evidence-based and others experimental, designed to improve maternal health and well-being and improve the distribution and retention of the workforce.23 Variable success over time prompted the creation of the 2022 White House Blueprint for Addressing the Maternal Health Crisis, Goal 4 of which specifically addresses the expansion and diversification of the perinatal workforce.24 The blueprint calls for expanded training of OB/GYNs, FMS, CNMs, and NPs, with emphasis on representative diversity (Goal 4.1 and 4.2). The blueprint also calls for expanding doula services and free-standing birth centers (Goal 4.4).24
Place-based education is one highly effective strategy for improving recruitment, retention, and distribution of the health care workforce.25 North Carolina continues to expand medical schools and residency programs, including programs that offer rural tracks or rural training emphasis. North Carolina is home to nine OB/GYN residency programs, currently graduating 49 physicians per year.17 The most recent program opened in 2018 in Fayetteville, North Carolina. Overall, only 20%–50% of graduates from these programs began practice in North Carolina; however, the vast majority remained in practice in North Carolina after five years.26
Other residency programs, most notably for FM, offer Rural Training Track (RTT) programs with significant educational training in rural locations (e.g., see https://www. acgme.org/what-we-do/accreditation/medically-underserved-areas-and-populations/rural-tracks/); these programs have been successful in improving the number of FMs practicing in rural counties.25 Recently, RTT programs have expanded into other medical specialties, and there are now several relatively new such OB/GYN programs in the United States, though none exist currently in North Carolina. However, this may change in the near future (Arthur Ollendorff, MD, President, Association of Professors of Gynecology and Obstetrics, text communication, September 6, 2022).
North Carolina is home to only 1 of the 43 US nurse-midwifery programs accredited by the Accreditation Commission for Midwifery Education. The program is located in the metropolitan area of the largest, mostly rural Eastern AHEC region.27 The top five North Carolina programs for women’s health or family NPs are located in large metropolitan areas in the AHEC regions of Wake, Greensboro (2), South East, and Eastern.28 While positioned to graduate many CNMs and NPs for potential entry into the North Carolina maternal health care workforce, these APPs may struggle to find employment opportunities, especially in rural areas. North Carolina continues to require a collaborative practice agreement with physician supervision for all CNMs and NPs, which may prompt some graduates to eschew practice in the state.
Another consideration nationally is the overwhelming trend toward female providers in maternity care. For women in particular, common themes associated with successful rural practice retention include spouse/partner fit, family ties, training experience in the community, social networks, shared community ideology, and support for development of a professional identity as a “rural physician”.25,29 Other highlighted recruitment priorities for women physicians considering rural practice include flexible scheduling, family leave, and child care.25
Strategies Specific to Western North Carolina
Proven approaches to advancing recruitment and retention of rural health care providers have not been developed. Rural representation in policy decision-making bodies at local, state, and federal levels—as well as in clinical and professional organizations, including maternal mortality review committees—has been suggested as one effective adjunct. In North Carolina, the AHEC system has fostered inclusion of rural providers in medical society leadership (both regional and statewide), state politics, and medical school expansion. Representation offers a potential avenue to payment reform, which in turn may support retention since more than half of rural patients are enrolled in Medicaid, which contributes to financial instability in medical systems, due to lower reimbursement rates.30
Efforts in Western North Carolina, specifically through MAHEC, have focused on both medical trainees and faculty. Although a rural track hybrid program for OB/GYNs was developed recently, it was not approved by ACGME; efforts continue across counties and multiple major medical systems to rework and resubmit this application. An OB/GYN resident position for expected graduation in 2026 was added, despite the CMS cap on positions; it is currently funded within a HRSA training grant. There is also an accredited maternal-fetal medicine fellowship currently in its second year, one of only a few nationwide sponsored by a community program. Additionally, a first-year faculty is experiencing practice as a rural physician as part of a rural fellowship in women’s health sponsored through HRSA funds.
A number of different provider types train at MAHEC and our hospital affiliate, including CNMs, NPs, and medical students, as well as residents and fellows in a wide range of disciplines, including emergency medicine. FM continues to provide obstetric training for all residents and includes both low-risk continuity outpatients and integration into the obstetric hospital team for high-risk exposure and deliveries. There is a robust presence of CNMs who provide care and resident supervision for low-risk patients, including through delivery and postpartum.
Community engagement remains a regional priority. An extensive doula program assists our Medicaid population throughout pregnancy, lowering social stress and increasing support for patients and providers. Support for regional providers includes a women’s health toolbox containing easily accessible and concise information on important national recommendations for obstetric care. MAHEC also hosts a quarterly African American Health Webinar Series, now in its second year, which culminates in the Asheville African American Health Symposium and has included segments on women’s health. Both the webinar and symposium feature national experts helping to combat health care oppression and disparities. Additionally, our simulation center hosts regular training for women’s health providers, labor and delivery staff, and emergency department health care workers.
Finally, but importantly, MAHEC has placed a major emphasis on improving recruitment of a diverse resident and faculty workforce. Since 2005, the Minority Medical Mentoring Program (MMMP) has paired underrepresented-in-medicine high school seniors with a varied group of local health care professionals in a semester-long internship for honors course credit. MMMP has contributed directly to the regional health care pipeline. Direct connection to historically Black colleges and universities (HBCU) has increased the number of applicants and residents from groups typically underrepresented in medicine. An organization-wide commitment to diversity and equity in a recent website redesign and all documents has also expanded representation.
In conclusion, no one approach will guarantee effective recruitment and retention of a highly skilled, diverse, inclusive workforce, particularly as the instability of hospital closures and women’s health services, such as labor and delivery, continues. Effective efforts will require emphasis on local training opportunities, community connection, and employer flexibility, along with reassessment of policy and fiscal issues.
Disclosure of interests
The authors are employed by MAHEC and disclose no further interests.