Background
North Carolina has the 20th-highest rate of maternal mortality in the United States, with a rate of 20.6 maternal deaths per 100,000 live births in 2018–2020.1 Maternal health is intimately interconnected with infant health. Approximately two out of three pregnancy-related deaths occur during the first 42 days postpartum—the first half of the “fourth trimester”.2 New families need support, information, and resources to navigate postpartum recovery and early family formation and to achieve biopsychosocial and economic well-being. Education for health care team members, mothers and birthing people,[1] families, and communities is key to reducing maternal mortality.
In 2021, the Centers for Disease Control and Prevention (CDC) review of data from 36 Maternal Mortality Review Committees (MMRCs) found that 80% of pregnancy-related deaths were preventable.3 North Carolina is one of 31 states receiving funding from CDC Enhancing Reviews and Surveillance to Eliminate Maternal Mortality (ERASE MM). These funds provide the opportunity to identify factors contributing to maternal mortality, pregnancy complications, and the associated disparities in health care among different ethnicities and sociodemographic groups. A portion of North Carolina’s funding supports educational initiatives, such as the “I Gave Birth” initiative at ECU Health, which provides education on maternal warning signs and emergencies.
ECU Health Medical Center is the flagship academic medical center for ECU Health, located in Greenville, North Carolina. It is a Level 1 Trauma Center and a Level 4 Birthing Facility as defined by the American College of Obstetrics and Gynecology. As a Level 4 Birthing Facility, ECU Health Medical Center provides maternal and neonatal outreach to regional facilities.
The “I Gave Birth” initiative focuses on increasing access to resources and support needed to navigate the early postpartum period. The overall goal of reducing maternal mortality starts with small steps. The general public and medical personnel who do not routinely see birthing people lack knowledge of complications that can occur following delivery. Access to such knowledge is key to reducing maternal mortality and morbidity. A bracelet given to individuals after giving birth serves as a visual reminder to the birthing person of the potential complications of the postpartum period, while also alerting medical personnel of the unique care needs of the postpartum patient. Providing standardized education to health care professionals enhances the care that women of childbearing age receive. Heightening awareness of the warning signs of postpartum risks facilitates prompt recognition of post-birth complications, which can decrease maternal mortality with time. Educated patients are empowered to take an active role and be an advocate in their birthing journey.
Education
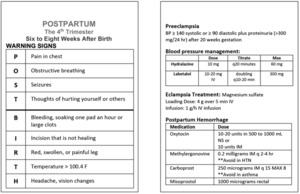
The “I Gave Birth” bracelet initiative is designed to educate health care team members not specializing in maternal health about the unique warning signs surrounding the fourth trimester. For example, a patient presenting to the emergency department with a blood pressure of 140/90 may not routinely alert emergency medical personnel to take immediate action. However, this blood pressure reading can be dangerous for a postpartum patient.4 The initiative was developed to build upon the concepts taught in the Association of Women’s Health Obstetric and Neonatal Nursing (AWHONN) Post-Birth Warning Signs training.5 The regional Perinatal Nurse Champion (PNC), in collaboration with the ECU Health Perinatal Outreach team, provided education for pre-licensure professionals, emergency medicine, and family medicine residents at ECU Brody School of Medicine, and nurse-midwifery students at the ECU College of Nursing. The education included Advanced Life Support in Obstetrics (ALSO), awareness of post-birth warning signs, and the “I Gave Birth” bracelets. Additionally, medical students created a post-birth card to provide a quick reference guide for the care of patients in their fourth trimester (Figure 1).
Hospital Implementation
An interdisciplinary team at the hospital level was organized to support implementation of the “I Gave Birth” bracelet initiative within ECU Health. Led by the PNC, the team was comprised of the labor and delivery nurse manger, postpartum nurse manager, nursing educators, data managers, and the ECU Health Obstetric Medical Director. The team developed a timeline and process for educating staff and patients. The SOAP note (subjective, objective assessment plan) format was utilized to communicate to all team members during the planning phase. The dissemination of education and information to ECU Health nursing staff took place during shift huddles and via emails. Upon completion of the education, workflows and procedures were created to support implementation.
From August to November 2021, patients who delivered at 20 weeks or greater gestation received the “I Gave Birth” bracelets and the post-birth warning signs education, including those who suffered a fetal or infant loss. The PNC and unit managers from mother-baby and labor and delivery units completed manual bracelet counts to verify that the bracelets were distributed. To verify the implementation process, metrics were reviewed utilizing the support of the Quality Nurse Specialist. A review of all medical records was completed to collect data on the distribution of bracelets and to identify patients readmitted to the hospital in the postpartum period. Job aids, such as EPIC smart phrases, were created to support documentation. These tools were disseminated facility-wide to unit managers. Presentations and trainings were provided to outpatient providers to support the transitions of care.
Regional Implementation
As the only tertiary care center in the 29 counties that make up Perinatal Region VI, ECU Health Medical Center is instrumental in sharing best practices and quality improvement activities, such as the “I Gave Birth” initiative. The implementation team presented the initiative to ECU Health facilities and other birthing facilities within Perinatal Region VI after implementation was sustained at ECU Health to support improvement at those facilities, as well as transitions of care for critically ill postpartum people. In addition, education and training were provided to the Emergency Management Services within this region, including education on maternal warning signs and information about the “I Gave Birth” bracelets and their meaning. “I Gave Birth” bracelet flyers were placed in offices providing prenatal care and the obstetrical units across the region to enhance health care provider and patient awareness (Figure 2).
Outcomes
Data collection on bracelet distribution, postpartum readmission, and the number of patients wearing “I Gave Birth” bracelets to postpartum appointments were a few of the points assessed. Of note, obstetrical-related readmissions fell from 2.24% in 2019 to 1.47% in 2022 for ECU Health Medical Center (internal data). It is thought that this decrease of 0.77% has a direct correlation with the implementation of the aforementioned education provided to patients, family members, and medical personnel, which contributed to the provision of risk-appropriate care. Patients in this cohort appear to be seeking care and receiving timely treatment.
Initial qualitative interviews revealed patients’ understanding of the importance of receiving care during the immediate postpartum period. The PNC had the opportunity to engage with individuals in the community who had given birth recently. An assessment was completed to determine the effectiveness of patient education about both the bracelet and maternal warning signs education. Respondents were able to recall and share the purpose of the bracelets as a visual cue, as well as the importance of seeking help during the postpartum period. Additionally, health care team members within the hospital and medical offices noted an increase in the number of individuals returning with bracelets. Regional emergency care workers verbalized an increase in knowledge related escalation of care during the postpartum period.
Discussion
The “I Gave Birth” bracelet initiative provided an opportunity to enhance communication between hospital departments, health care team members, birthing people, families, and communities. Individuals seeking emergency services wearing these bracelets received life-saving medications within minutes of seeking care. By the end of September 2021, providers began seeing postpartum patients wearing their “I Gave Birth” bracelets during outpatient appointments. Providing interprofessional education that reached across ambulatory and inpatient settings strengthened the care provided. Interest in replication of this initiative has risen across North Carolina. During the 2022–2023 grant cycle, the “I Gave Birth” initiative will be expanding to facilities in Perinatal Regions I, II, and IV.
For communities seeking to implement this initiative, it is crucial to take into consideration the development of strategies and workflows for providing care for those who have experienced a perinatal loss. Those experiencing a fetal death after 20 weeks remain at risk for illness in the postpartum period, but may not desire to wear a bracelet alerting others of their recent loss. In this population, it is imperative that post-birth warning signs awareness and education be emphasized and properly tailored.
Conclusion
Being proactive and not reactive during a time when birthing persons need not only prenatal and labor care but also a focus on postpartum care is imperative. The magnitude of the epidemic of growing maternal mortality is difficult to grasp. An initiative like “I Gave Birth” provides education to those providers who do not routinely interact with pregnant or postpartum individuals, while also increasing general community awareness and knowledge of maternal warning signs, and this approach has the potential to impact the maternal mortality rate in North Carolina. The hope is that additional sites will utilize a similar process to implement such initiatives to educate providers, patients, and families; heighten awareness of warning signs; and support risk-appropriate care that enables escalation of care during the postpartum period, therefore improving the health of mothers and birthing people in North Carolina.
Disclosure of interests
The authors report no conflicts of interest.
We are striving to use language inclusive of all genders with the recognition that full equity and inclusiveness have not yet been achieved. To promote inclusivity, and out of respect for the diversity of identities of those who reside in North Carolina who are pregnant and give birth, the terms birthing person, mother, pregnant women, and pregnant person are being utilized.