Introduction
The coronavirus pandemic forced health care providers to rethink and quickly reinvent the delivery of care to patients, particularly in rural settings. Fear of COVID-19 and the lack of definitive and timely information caused many patients to be no-shows at clinic appointments and, as a result, not receive the care they needed. This posed an especially critical challenge for the maternal, fetal, and newborn population in the 29-county area that East Carolina University (ECU) serves. ECU, the safety-net provider for 1.4 million people in Eastern North Carolina, is the only source for high-risk prenatal care in the region. COVID-19 exacerbated an already dire situation for the health of expectant and new mothers in Eastern North Carolina.
The data on health care disparities from the 41 North Carolina counties along or east of the I–95 corridor are stark. The premature mortality rate for the region is 18% higher than for the state overall.1 Diabetes mortality is 29% higher, and the diabetes mortality rate for non-White females in the region is more than double the rate for White females in the state overall.1 The poverty rate is 17%, compared to 14% for the state; the child poverty rate is 25% and 18 of the counties in the region have a child poverty rate over 30%.2 Fifteen percent of the population is food insecure, and many in the largely rural region have low access to a food store.3 For 18 of the counties in the region, 70% or more of the births were to mothers with Medicaid.4 Socioeconomic factors in the region limit access to transportation, adequate nutrition, and basic necessities for the maternal population.
On a larger scale, the United States has unacceptably high maternal and infant mortality rates, especially for African American and American Indian mothers. Several factors contribute to this health disparity, including prevalence of underlying conditions, racism-induced stress, unconscious bias in health care, and lack of quality prenatal care.5 Nationally, more than 700 women die each year of complications related to pregnancy and two-thirds of these deaths are preventable.6 As of 2016, the US pregnancy-related mortality ratio was 16.9 per 100,000 live births.7 For North Carolina, the rate was 20.7.8 However, there are significant racial disparities within these calculated statistics. In the United States, for non-Hispanic White women, the ratio was 14.1 deaths per 100,000 births, whereas for non-Hispanic Black women it was 41.4, and for American Indian/Alaskan Native it was 26.5.7 Within North Carolina the rate for non-Hispanic White women was 15.9, and for non-Hispanic Black women it was 27.7.8 There is also a large racial disparity in infant mortality. The total infant mortality rate for the United States was 5.6 deaths per 1000 births, but the rate was 4.5 for non-Hispanic Whites and 10.6 for non-Hispanic Blacks.9 For North Carolina, the total infant mortality rate was 6.9. In the northeastern perinatal region of the
state, which most closely corresponds to Eastern North Carolina, the total infant mortality rate was 9.2, while the non-Hispanic White rate was 6, and the non-Hispanic Black rate was 15.3.10 These data demonstrate that maternal mortality and infant mortality disproportionately affect Black and American Indian/Alaskan Native women and infants in the United States and in North Carolina. Additionally, there are disparities between rural and urban populations.11 According to publicly available data from the US Centers for Disease Control and Prevention (CDC) and analyzed by Scientific American, rural areas had a pregnancy-related mortality ratio of 29.4 per 100,000 live births versus 18.2 in urban areas in 2015.12 COVID-19 highlighted these disparities in health outcomes even further.13
Maternal mortality is due to a confluence of factors, not all of which stem from within the clinical walls. These factors include social determinants of health; disproportionate rates of preexisting health conditions; limited access to health care, including high-quality prenatal care; and the role of pervasive racism. All of these factors contribute to disparate health outcomes for Black and American Indian/Alaskan Native (AI/AN) women and their families.
Mental health is also a key factor in overall maternal health and well-being. Perinatal mental health conditions, such as anxiety and depression, are very common complications of pregnancy, affecting roughly 8%–11% of all women during pregnancy and 6%–12% in the postpartum period.14 Perinatal mental health conditions are more common for African Americans, and also for low-income women.14 The COVID-19 pandemic has also increased the incidence of perinatal anxiety and depression, due to social isolation, difficulties accessing care, and increased economic insecurities.15 Mental health screenings during prenatal visits are an established method for identifying women in need of additional care,16 but to be effective, screenings must be integrated into routine care, and follow-up care must be available. Yet, mental health services, and especially psychiatric services, are often hard to find in low-income, minority, and rural areas, where the need is highest. Indeed, 94 of the 100 counties in North Carolina are designated as mental health provider shortage areas, and Eastern North Carolina has a disproportionate share of these underserved counties.17
MOTHeRS Project: Outreach Through Telehealth
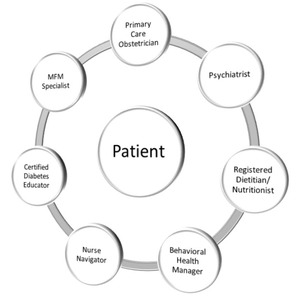
In July 2020, ECU expanded the North Carolina Statewide Telepsychiatry Program (NC-STeP)—a statewide telepsychiatry program founded by the first author (S.A.S.) nearly a decade ago—to bring multidisciplinary care to three community-based primary care obstetric clinics in Carteret, Duplin, and Chowan counties.18–20 A fourth site at Dare County was added in September 2022. The MOTHeRS (Maternal Outreach through Telehealth for Rural Sites) Project brings the primary obstetrician together with multiple aspects of patient care, including a maternal fetal medicine specialist (MFM), a psychiatrist, a diabetes educator, a behavioral health manager, and a nurse navigator. Telepsychiatry is an essential element of the MOTHeRS Project. Every patient is administered two mental health screening tools: the nine-question Patient Health Questionnaire (PHQ-9) and the seven-question GAD-7. Patients who screen positive for a mental health condition are referred for a tele-consult with the behavioral health manager and, if needed, are referred for a consult with the telepsychiatrist for additional follow-up, typically within the same clinic location. Telepsychiatry offers a potential approach for enhancing maternal health care by linking the maternal health practice with an offsite psychiatrist in an integrated care model. In this way, mental health care is embedded within the clinic, with the clinic doctor retaining primary management of the patient while the telepsychiatrist provides specialized care as needed.21
The psychiatrist provides four remote hours of consultation time to each clinic per week. The general obstetrician also refers high-risk patients to tele-consults with an MFM based at ECU where appropriate. Ultrasounds are conducted at the primary clinic location and transferred electronically along with other electronic health records prior to the MFM specialist visit. High-risk pregnancies can exacerbate depression and anxiety, so pairing maternal health with mental health care serves the physical and mental well-being of these pregnant patients. When indicated, patients can be referred for a tele-consult with a registered dietitian and a
certified diabetes care and education specialist. A nurse navigator coordinates the process. The behavioral health manager coordinates the mental health care, and the primary obstetrician remains the overall coordinator of care and the prescriber. The components of the MOTHeRS Project are illustrated in Figure 1.
The association of food insecurity (FI) and diet quality with mental health and poor outcomes in high-risk pregnancies has been established by experts. Interprofessional interventions, including addressing FI, are known to relieve stress and depression.22–25 The MOTHeRS Project protocol includes screening all patients at its clinical sites for FI. A validated, two-item tool widely used in other clinical settings is used,26 and those screened as food-insecure are offered a medically tailored food bag, printed nutrition education, and links to existing community resources for emergency food. Essential nutrients contributing to a healthy pregnancy that are often under-consumed and not adequately covered with a prenatal vitamin supplement were identified and included in the food bag; items included in the MOTHeRS food bag are a good source of at least one of the identified target nutrients. The bag supplies nutritional needs of a pregnant woman for two weeks on its own, or four weeks with WIC. Items used are shelf-stable, affordable, readily available at a local grocery store, and well-received and utilized by the target population, as well as being appropriate regardless of trimester or comorbidities and complementary to WIC Food Package V. The details are available at http://hdl.handle.net/10342/9073.27,28
Women at the first clinic—Carteret Ob-Gyn Associates—participated in a qualitative study to examine their experience, satisfaction, and utilization of the food and nutrition education resources provided. The program did address gaps to food access in other traditional community-based food assistance programs, such as SNAP and WIC. Addressing FI helped alleviate strain and stresses for already vulnerable households. The stigma surrounding traditional food assistance programs seemed lightened by the provision of emergency foods in a clinical setting. Those participating in the interviews reported high satisfaction with the food bags and educational materials.25
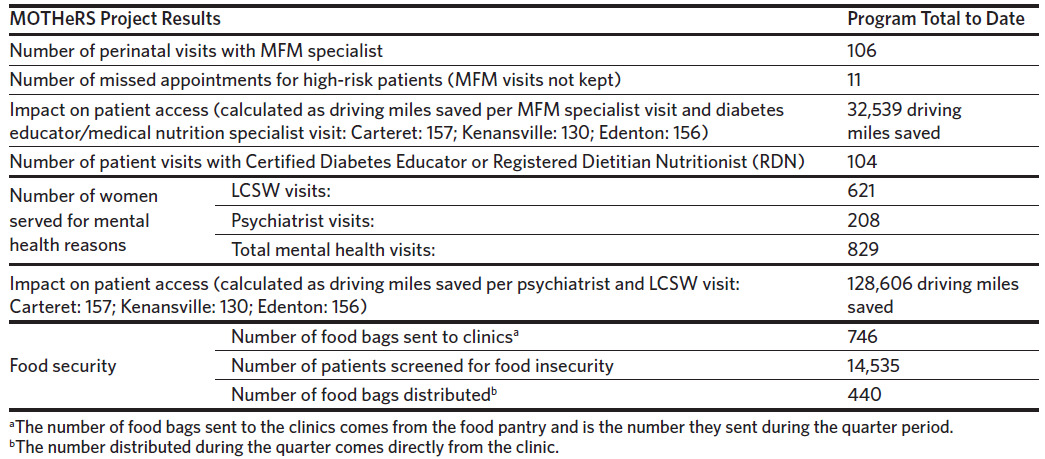
Through the MOTHeRS Project’s formalized partnerships at the clinical sites, patients in the practices are cared for by both an MFM specialist and their local OB-GYN physician through a combination of telehealth and face-to-face visits. This model helps manage patients in clinics closer to their homes and minimizes travel to the remote specialty clinics for high-risk patients, such as those with diabetes, chronic hypertension, opioid/substance use, and/or psychiatric needs. Aside from enhancing access to services, this model helps to reduce geographic health disparities, enhances patient convenience, and improves patient adherence to treatment (Table 1). By bringing specialists to the primary care sites, this model also reduces professional isolation, enhances recruiting and retention of health professionals in underserved areas, and improves coordination of care across the health care system.
The first clinical site for the project, Carteret Ob-Gyn Associates, has been operational since mid-January 2021. Two additional sites in Chowan and Duplin counties went live in July 2022. A fourth site in Dare County went live in September 2022. All four sites now have all equipment for telehealth in place, with providers and staff trained in use of the equipment and its integration with the electronic health record (EHR). Providers are credentialed and their schedules are already built into the EHR. A new ultrasound machine for one of the sites was purchased and it is integrated with PACS (picture archiving and communication system) to enable the MFM specialists to see images remotely. PACS is a medical imaging technology used primarily in health care organizations to securely store and digitally transmit electronic images and clinically relevant reports. Counseling for gestational diabetes is accomplished through telehealth visits as well.
Conclusions
Despite high health care spending, the United States has some of the worst maternal outcomes in the industrialized world.29–32
The collaborative co-management model used by the MOTHeRS Project creates a patient-centered team approach to care delivery that results in both improved patient experiences and a positive impact on maternal-fetal health. The model also has the flexibility of providing telehealth services directly to patients in their homes from their tablets, computers, or smartphones, if clinically indicated.
Evidence points toward disproportionately high maternal deaths of Black and other minority women, especially in rural areas. There are significant challenges facing rural women in accessing comprehensive, affordable, high-quality maternal health and mental health care. Given the scale and scope of the issue, we believe that programs like the MOTHeRS Project are very much needed and timely. The project emphasizes the importance of strengthening care coordination and health care delivery, investing in human services programs, and addressing various workforce issues. Although
there are numerous programs that have been developed to improve maternal health outcomes, barriers such as persistent poverty, transportation challenges, lack of affordable quality health insurance, chronic health conditions, and workforce shortages have made it difficult to address a complex issue such as rural maternal health care. Through its ongoing work, the MOTHeRS Project expects not only to provide care to those who need it at its clinical sites, but also to generate new knowledge regarding how these barriers can be better addressed to ensure that every woman in rural America has a safe and healthy pregnancy, delivery, and postnatal outcome.
Acknowledgments
Financial disclosures. The MOTHeRS Project is supported by a generous gift from the United Health Foundation. The North Carolina Statewide Telepsychiatry Program (NC-STeP) is funded through a blend of state, philanthropic, and federal funds. In addition to the North Carolina General Assembly appropriation of $1.82 million per year to fund the program, NC-STeP is partially funded by The Duke Endowment (which copublishes the NCMJ), Fullerton Foundation, BCBS Foundation, and HRSA. HRSA is also allowing the North Carolina Office of Rural Health (ORH) to use a portion of federal Flex funding to cover some unfunded ORH costs to administer the NC-STeP program. The North Carolina Department of Health and Human Services provides administrative oversight of the funding.
The authors have no conflicts of interest to declare. We are also grateful to the editors for their constructive feedback and support.