The ongoing collection, detection, monitoring, and reporting of emergency department (ED) data for COVID-19-like illness syndrome (CLI) plays an important role in public health disease surveillance.1–3 Examining trends of CLI using ED data can provide the basis for informing decision-making for public health officials, health care providers, and policymakers.4,5
In 2004, the North Carolina Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT) was established as the state’s premier population-based syndromic surveillance system.6 As of July 2020, 126 hospitals in North Carolina were submitting ED visit data to NC DETECT, accounting for over 99% of all ED visits in the state. The North Carolina Department of Health and Human Services (NCDHHS) relies on NC DETECT and other data sources to continuously monitor CLI and other respiratory diseases across the state (and 7 public health regions).6 Given the robust monitoring and reporting of county-level rates and patient demographics (e.g., age groups, race) by state data dashboards of CLI, there are a limited number of peer-reviewed studies in the literature on CLI-related ED visits and none to our knowledge that have been published using North Carolina syndromic data.
The primary purpose of this project was to examine regional trends of CLI-related ED visits across North Carolina during the initial phases of the COVID-19 pandemic. These findings offer useful information for estimating the magnitude and distribution of CLI-related ED visits while stimulating research and informing public health policy.
Methods
This project was a collaboration between East Carolina University (ECU) Brody School of Medicine and Research Triangle Institute (RTI) International. All Institutional Review Board (UMCIRB #20-002847) and data use agreements (NCDHHS) were approved prior to receiving any data for this study.
Inclusion criteria for cases were defined as all eligible North Carolina resident patients who had an ED visit in the state between March 1, 2020, and November 30, 2020, and who met the NC DETECT and North Carolina Division of Public Health’s constructed syndromic surveillance case definition for “COVID-like illness”.7 Note that while CLI definition now includes ICD-10-CM codes, these codes were not introduced during the early weeks of the pandemic and were not available from NC DETECT for the project study period at the time of our data request. For this project, a CLI-related ED visit was defined as the unit of analysis and having met 1 or more of the following: 1) Chief complaint only: “COVID” or “corona” or “coronavirus;” or chief complaint or triage notes: “loss of sense of smell” or “taste or no taste” or “smell or unable to smell” or “taste or loss sense of smell” or “taste or lost taste” or “smell”; 2) Chief complaint or triage notes: “cough” or “shortness of breath” or “SOB” or “SHOB” or “respiratory distress” or “cannot breathe” or “cyanosis” or “difficulty breathing” or “dyspnea” or “hypoxia” or “pleural effusion” or “pneumon” or “stridor;” and “febrile” or “fev*” or “fvr” or “temp” or “chills” or “rigor” or “shivers” or initial ED temp > 38o Celsius".6
ED visits by patients who were not North Carolina residents or did not meet the CLI case definition were excluded.
North Carolina Regions
The study area included all North Carolina counties (N = 100) and facilities reporting to NC DETECT. CLI-related ED visit trends were assessed by separating North Carolina counties into 3 well-established geographical regions: Eastern (n = 41 counties), Piedmont (n = 35 counties), and Western (n = 24 counties).
Measures
Available NC DETECT data variables used to describe sociodemographic characteristics of interest included patient age (categorized as 0–17, 18–24, 25–49, 50–64, 65–74, and > 74 years), sex (male, female), race (White, Black, American Indian, Asian, Pacific Islander, and Other), and ethnicity (Hispanic, non-Hispanic).
Other available data variables of interest included insurance type (e.g., insurance company, self-pay, Medicare, Medicaid, worker’s comp, other government, other, and no charge), and ED disposition (admitted to hospital floor bed and all other ED disposition options).
Weekly counts of CLI-related ED visits were determined by patient county of residence and by region. County-level rates of CLI-related ED visits were calculated using population estimates for each North Carolina county. Unadjusted rates were calculated by age groups using CLI-related ED visits as the numerator and 5-year population estimates for North Carolina, obtained from the US Census Bureau American Community Survey (2015–2019) as the denominator.8,9 Estimates were divided into quantiles, and mapped using ArcMap 10.7.1 (ESRI, Redlands CA).
Data Analysis
Patient characteristics derived from ED data were evaluated using frequencies and percentages for categorical variables and medians with the interquartile range for continuous variables. Univariate analysis was used to calculate frequency distributions, means, and standard deviations. Graph timelines of CLI-related ED visits were produced and examined over the entire study period and discussed among the investigating authors. Data analysis was performed using SAS Enterprise Guide. 7.1 (SAS Institute, Cary, NC).
Results
As shown in Figure 1, from March 1 to November 30, 2020, there was a total of 2,996,751 ED visits reported to NC DETECT. After applying inclusion/exclusion study criteria, a total of 133,193 CLI-related ED visits remained and were evaluated for the study period.
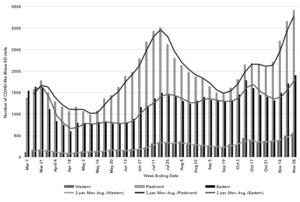
As shown in Figure 2, the overall trend lines of CLI-related ED visits across the 3 regions were comparatively similar but with some variation between the number of weeks over the entire study period. Overall, the Piedmont region experienced the greatest number of reported CLI-related ED visits and largest trend variations. Similar but less dramatic varying peaks and troughs were observed within a few weeks of the same time frame in the Eastern and Western regions. All regions experienced a decline in the initial weeks (late March and early April) of the pandemic, and later in mid-September. Several notable peaks were observed with the first steady incline occurring from early May to July in the Piedmont region followed by a second peak from late October to late November (end of the study period).
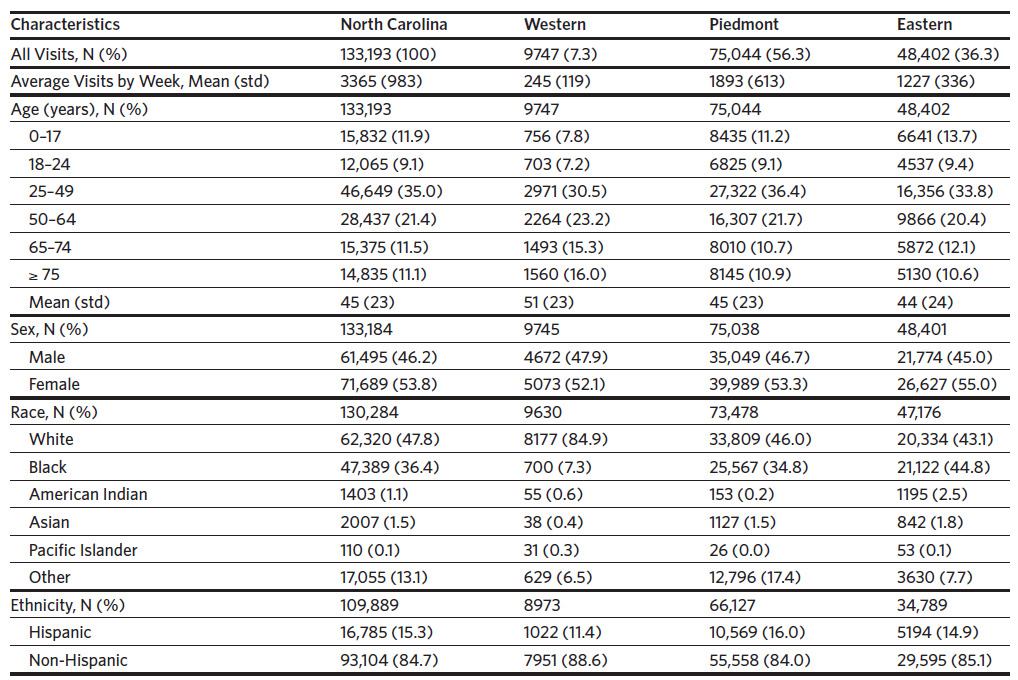
As shown in Table 1, the highest volume of CLI-related ED visits was reported in the Piedmont (56.3%), followed by the Eastern (36.3%) and the Western regions (7.3%). Compared to the Piedmont and Eastern CLI-related ED visit patient population data, Western patients tended to be older (aged 51 years versus 45 years and 44 years, respectively).
The 25–49 age group had the highest percent (35.0%) of reported CLI-related ED visits while those aged 18–24 years had the lowest. Age groups with the largest reported CLI-related ED visits were 25–49 in the Piedmont, 0–17-in the Eastern, and aged 50 and older in the Western region. For ethnicity of CLI-related ED visits, the largest percent Hispanic individuals were reported in the Piedmont (16.0%), while the East reported the highest number of American Indian individuals (2.5%).
Across all regions, CLI-related ED visits were higher among women than men (53.8% versus 46.2%). Nearly twice as many CLI-related ED visits occurred among White residents in the West (84.9%), compared to the Piedmont (46.0%) and Eastern (43.1) regions. More CLI-related ED visits were made by Black residents in Eastern counties (44.8%) compared to the Piedmont (34.8%), and Western (7.3%) regions.
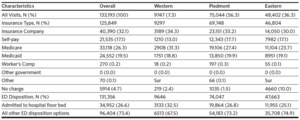
As shown in Table 2, a slightly lower percent (30%) of CLI-related ED visits in the Eastern region reported “private insurance company” as source of payment compared with the Western (34.3%) and Piedmont regions (33.2%). Ten percent (10%) of CLI-related ED visits in the East were reported as “no charge,” compared to 2% or less in other regions. Approximately 25% of CLI-related ED visits were reported in the Eastern region as being admitted to the hospital, which compared similarly to the Piedmont region (26.8%) but was considerably lower than the Western region (32.5%).
When rates (per 100,000 population) were calculated (Figure 3), counties in the Eastern region experienced the highest CLI-related ED visit rates in the entire state (i.e., Hertford, Bertie, Edgecombe, Martin, Chowan, Tyrrell, Washington, Martin, Edgecombe, Nash, Wilson, Pitt, Greene, Lenoir, Duplin, Sampson, Wayne, Robeson, Hoke, and Scotland counties). In the Piedmont region, Richmond, Anson, Montgomery, and Lee counties had the highest rates while Wilkes, Caldwell, and Cleveland counties had highest rates in the Western region.
Discussion
Over the initial 9 months of the pandemic, CLI-related ED visits across the 3 regions of North Carolina followed comparatively similar trends with some temporal variation (i.e., weeks) between peaks and troughs. Factors that gave rise to these patterns are important to understand but somewhat difficult to interpret with accuracy given the many other conditions surrounding the pandemic, which were outside the scope of this study.
In general, ED visits were reported to have significantly declined globally following policy implementation measures to reduce disease transmission (i.e., stay-at-home orders, school and business closures, and messaging to encourage staying at home).10 This was consistent with our findings that identified declining trends in CLI-related ED visits in late March and early April, shortly after COVID-19 had been detected in the United States. Several other North Carolina studies using syndromic data reported similar results. Harmon and colleagues found reduced ED visits for injuries while Wong and colleagues demonstrated fewer myocardial infarction and stroke ED visits during the initial phases of the pandemic.11,12 These findings support the impacts that policy had on society’s decisions about whether to seek ED care.10
As a descriptive study, the authors were able to glean that rural areas reported higher numbers of CLI-related ED visits and rates particularly among Black residents in the East, White and elderly residents in the West, and younger adults (29–49 years) in the Piedmont region.
While the highest volume of CLI-related ED visits occurred in the Piedmont, Black residents in the Eastern region had considerably more CLI-related ED visits when compared to the rest of the state. During the same time frame as our study, nearly twice as many new COVID-19 cases were being reported from rural North Carolina counties compared to urban and suburban counties.13,14 Furthermore, most Eastern counties—specifically Bertie, Hertford, Northampton, Edgecombe, and Halifax counties—are largely impoverished with a significantly high proportion of Black residents, characteristic of the health disparities in the region. Access-to-care issues, including limited health care providers, scant transportation options, and use of the ED as a “safety net” care option, are certainly plausible and well-documented contributing factors for poor, rural areas.15,16
In the Western region, the highest percent of CLI-related ED visits was among White and elderly residents in 3 rural counties (i.e., Wilkes, Caldwell, Cleveland). This was somewhat surprising given the high-risk status of seniors and limited health care options in rural areas.17 As previously mentioned, the use of the ED as a safety net was a likely consideration for more visits. However, noticing that these counties bordered suburban counties and a review of the literature provided more insight. Findings from a systematic review by Dufor and colleagues (2019) reported that rural, geriatric patients living near urban areas were more likely to seek care at the ED for a number of reasons, including having a high number of previous hospital and/or ED admissions, reporting a high number of prescribed drugs, being of low income (Medicaid beneficiary), or having a history of heart disease.18 Any or all of these factors appear to be valid reasons, though given these studies were conducted outside of a pandemic situation, they deserve a more thorough examination. Despite an overall increase in the supply of physicians in North Carolina in recent years, rural areas continue to struggle with access-to-care issues. Rural counties in North Carolina have poorer access to health resources, including hospitals, and half the number of physicians (per 10,000 residents) as urban counties.18–20 Policy action to address these issues should remain at the advocacy forefront for rural North Carolina counties.
In general, the majority (35%) of CLI-related ED visits occurred in the 25–49 age group. While this age group represents the largest percent of the population in North Carolina, other reports indicate that this same age group also experienced higher COVID-19 cases during the same time frame as our study period.14 According to national data, during the first year of the pandemic (approximately May to October, 2020) the median age distribution shifted considerably from elderly to young adults (an estimated 76% of cases or approximately 7 million people).21,22 While social behavior (e.g., engaging in close contact sports, going to bars, traveling, attending unmasked get-togethers) is a primary risk factor for COVID-19 among young adults, individual variability and variant strains have also been cited.21 In a coronavirus study of adults by Monod and colleagues, those aged 20–49 years were the only age group with sustained COVID-19 transmission rates that continued to contribute to viral spread relative to their size in the population.23 Undoubtedly, more public health intervention strategies and efforts, such as social media immunization campaigns particularly targeted at this age group at universities, workplaces, sporting and entertainment events, should be considered.
Strengths and Limitations
The use of syndromic data to describe CLI-related ED visits provides an important and unique way of describing trends across the state.5 While surveillance systems have been shown to be highly useful, there are several inherent limitations when using syndromic data.24 In North Carolina, syndrome definitions are based on ICD-10-CM coding, patient’s chief complaint, and triage notes, but do not represent clinically confirmed disease.6 Although ICD- 10-CM coding is used for CLI, initial patient ED visit information is collected and often recorded in free text fields, which are subject to data-entry issues. While the CLI definition now includes ICD-10-CM codes, these codes were not introduced during the early weeks of the pandemic and were not available for this project at the time of our data request. Future studies of CLI-related ED visits in North Carolina should include a longer study period using the latest available data.
Conclusion
The ability to use syndromic surveillance data to monitor trends and patterns of ED visits across North Carolina remains vital to the understanding of health impacts on the population. Providing “real-time” laboratory monitoring and reporting is an additional way to improve and enhance COVID-19 surveillance efforts. As mutated strains of COVID-19 become widespread and other pathogens continue to emerge, syndromic surveillance data remain important to North Carolina health department leaders, hospital administrators, and policymakers when making informed decisions to protect our communities.25
Acknowledgements
The North Carolina Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT) is an advanced, statewide public health surveillance system. NC DETECT is funded with federal funds by a North Carolina Division of Public Health (NCDPH) Public Health Emergency Preparedness Grant (PHEP), and managed through a collaboration between NCDPH and the University of North Carolina at Chapel Hill Department of Emergency Medicine’s Carolina Center for Health Informatics (UNC CCHI). The NC Office of Emergency Medical Services (NC OEMS) and NC DETECT Data Oversight Committees do not take responsibility for the scientific validity or accuracy of methodology, results, statistical analyses, or conclusions presented. The findings and conclusions in this publication are those of the author(s) and do not necessarily represent the views of the North Carolina Department of Health and Human Services Division of Public Health.
The authors thank Bill Jones (formerly with NCDPH) and Amy Ising at NC DETECT for their valuable assistance with this project.
Funding
Funding for this project was provided by North Carolina House Bill 1043, 2020, COVID-19 Recovery Act.
Competing interests
The authors have no competing interests.

_emergency_department_(ed)_visits_data_flow_and_record_selection_p.png)


_emergency_department_(ed)_visits_data_flow_and_record_selection_p.png)