Injection drug use has significantly increased over the course of the opioid epidemic,1 contributing to the spread of many diseases, including hepatitis C virus (HCV),2 HIV,3,4 and infective endocarditis.5,6 Recent trends indicate that people who inject tend to be younger, white, unemployed, less educated, and live in rural areas.7 These geographically dispersed locations are characterized by limited transportation,8 high economic distress, and restricted access to health care providers, making it difficult to access substance-use-related services.
People who inject also report frequently being stopped by law enforcement officers,9 which has been shown to increase the likelihood of criminal justice involvement.10,11 Those who are arrested enter the “front door” of the system through admission to the county jail.12 There are currently 92 of these detention centers in North Carolina’s 100 counties and most (58%) have a maximum capacity of 200 or less.13 Despite their fairly small size, these jails collectively record more than 370,000 annual statewide admissions resulting in the confinement of 23,000 people at any time.14
Jails are primary intervention points for people with significant medical and behavioral health needs,15 yet a lack of systematic screening and assessment practices has led to extremely limited documentation of the prevalence of a variety of conditions.16 Most of the existing data collected from people in jails have been drawn from large metropolitan facilities, and the prevalence of drug injection has been estimated to be anywhere from 4% to 69% depending on the substance in question and the geographic location of the facility.17–19 The few studies conducted in rural areas have shown consistently high rates, with two-thirds to three-quarters of those admitted to jail reporting recent drug injection.20,21
Health conditions related to injection drug use are also complicated by the cycle of incarceration in rural areas.22 The average jail stay is approximately three weeks,23 a period too brief to deliver extended care yet long enough to destabilize employment,24 jeopardize housing,25 and increase stress,26 all of which can magnify the likelihood of readmission for a person with untreated substance use disorder (SUD), a condition shown to significantly increase the likelihood of repeated jail admissions.27
Considering the prevalence of injection drug use among people admitted to local jails, the potential for this high-risk practice to spread infectious disease, and the manner in which substance use contributes to incarceration,28 it is important to better understand the relationship between injection and jail readmission, especially among understudied populations in rural areas. The current study was designed to provide a detailed assessment of injection in two rural county detention populations. The relationships between injection, jail readmission, and length of time detained were examined to inform the adaptation of interventions to these special correctional settings.
Methods
Data and Measures
The key measures for the current study—injection drug use history and jail admission indicators—were drawn from a random sample of adults in two jails in Western North Carolina. These facilities are classified along with the majority of jails in the state regarding size and rural designation. According to the Federal Office of Rural Health Policy, both counties are categorized as nonmetropolitan.29 In terms of residential demographics, the populations are predominantly white (> 85%), about half are employed (55%), and most (90%) have completed high school or obtained a higher degree.30
Daily admission reports were used to generate random lists of participants over age 18 who were processed into the facilities within the past 96 hours over the course of a 12-month recruitment period. Participants were invited to conduct a structured interview, the Comprehensive Addiction and Psychological Evaluation-5 (CAAPE-5),31 which includes information related to demographic background, substance use, and mental health needs. This instrument takes approximately 40 minutes to complete and is consistent with the current criteria contained in the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).32
The project involved a 12-month observation period to assess the length of detention and jail readmission. Data regarding readmissions, charge severity, and detention duration were manually obtained for each participant from the facility’s records system. Readmissions were categorized with one group coded as having been readmitted on multiple occasions compared to a reference group of participants who were not admitted numerous times. Length of detention was recorded as the number of days detained during the follow-up period. These procedures were approved by the Institutional Review Board (protocol 977897-5).
Analysis
Descriptive statistics were calculated according to injection history. T-tests assessed continuous variables and chi-square analyses with corresponding p–values were used for categorical variables. A binary logistic regression model assessed the association between injection and the odds of multiple jail readmission occurrences during the study period while controlling for demographic background factors. Regression coefficients, odds ratios, corresponding 95% confidence intervals, Wald’s chi-square, and p-values were calculated for each covariate.
A second model assessed the association between injection and length of detention during the study period. Negative binomial regression was selected as most appropriate considering the count structure of the dependent variable and the probability of overdispersion.33 Regression coefficients, incident rate ratios, corresponding 95% confidence intervals, and p–values were calculated for each covariate in the model.
Results
The original study sample consisted of 442 participants. Preliminary analyses determined 22 were sentenced to more than one year in prison and became ineligible for follow-up assessment. The final sample included 420 participants aged 18–66 (mean age = 33.4). Approximately one-third (31.2%, n = 131) reported their gender as female and three-quarters (75.0%, n = 315) identified as white. Most (60.9%, n = 256) were unemployed immediately prior to incarceration and half (50.0%, n = 210) reported being single. The majority (90.0%, n = 378) of the sample was detained for a nonviolent misdemeanor offense.
In terms of SUD diagnoses, 70.9% (n = 298) met criteria for at least one SUD and 45.7% (n = 192) met criteria for multiple SUDs. Alcohol was the most prevalent substance with nearly three-quarters (70.5%, n = 296) of the sample exceeding the clinical threshold for a diagnosis. This was followed in sequence by over half (51.9%, n = 218) of the sample meeting criteria for methamphetamine use disorder, less than half (43.8%, n = 184) with cannabis use disorder, one-third (35.2%, n = 148) with opioid use disorder, and less than one-quarter presenting symptoms consistent with cocaine use disorder (21.4%; n = 90).
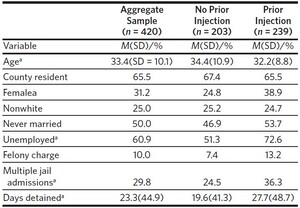
Injection drug use was defined as injecting drugs to get high in the 12 months prior to jail admission with slightly less than half (45.2%, n = 190) of the sample endorsing this item and the majority (71.6%, n = 136) reporting methamphetamine injection. Half (51.1%, n = 97) of those who injected reported injecting opioids. Smaller proportions of participants reported injecting cocaine (10.0%, n = 19) or another unspecified drug (7.9%, n = 15). Descriptive statistics according to drug injection are reported in Table 1. Participants who reported injection were younger on average, (t(418) = 2.28, p = .020), disproportionately female (χ2 (1) = 9.73, p = .002), and more likely to be unemployed (χ2 (1) = 19.88, p < .001) compared to those who did not report injection. Those who were admitted to the detention center on multiple occasions during the study period were also more likely to report injecting compared to those who were not admitted numerous times (χ2 (1) = 7.13, p = .008). Those who reported injection also spent an average of 8.1 additional days in the detention center during the 12-month follow-up period compared to those who did not inject, however, this difference was not statistically significant (Mdays injection = 27.7 - Mdays No injection = 19.6; t(418) = 1.84, p = .067).
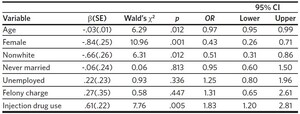
Logistic regression results are presented in Table 2. The estimated odds of multiple readmissions decreased for each additional year in participants’ age (OR = 0.97, 95% CI = 0.94–0.99). Additionally, female participants were less likely to be readmitted compared to their male counterparts (OR = 0.50, 95% CI = 0.30–0.83). Injection increased the probability of readmission, with those who injected being 1.83 times more likely to be admitted on multiple occasions during the 12-month study period compared to those who did not report injection (95% CI = 1.17–2.87).
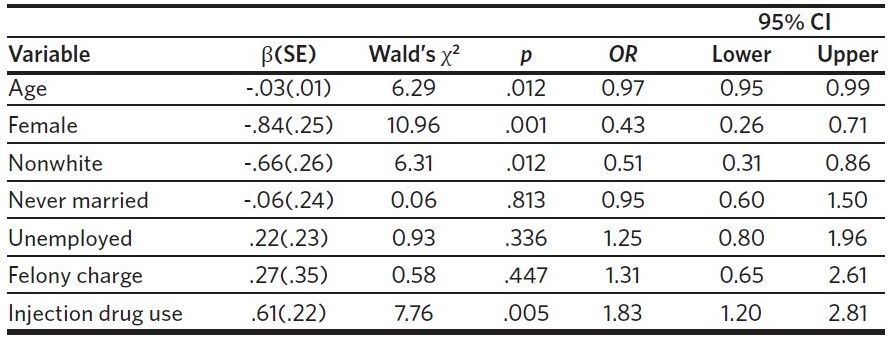
Several significant results were observed in the negative binomial regression model examining the length of time detained, presented in Table 3. Age was inversely related to the rate of days in detention (IRR = 0.98, 95% CI = 0.96– 0.99). Female participants experienced a significantly lower rate of days in detention compared to male participants (IRR = 0.60, 95% CI = 0.44–0.82). In addition, participants who identified with a racial or ethnic group other than white experienced a lower rate of detention days compared to those who did identify as white (IRR = 0.60, 95% CI = 0.43– 0.83). Injection was associated with a significantly higher rate of days in detention compared to those who did not inject (IRR = 1.34, 95% CI = 1.02–1.77). These results demonstrate that adults who reported injecting were not only more likely to be readmitted to the facilities numerous times during the 12-month study period, they were also likely to be detained longer compared to those who did not report a similar history.
Discussion
This study provides a detailed assessment of injection drug use in two understudied rural county detention centers. The observed relationship between SUDs and readmission converges with prior work.34,35 The nuanced analysis of the types of drugs injected in the current study indicated this result was largely driven by those who reported administering methamphetamine through this method.
This relationship between injection and readmission must be considered in a local context where most adults detained in rural county jails are residents of the community where the facility is located. The readmission rate of people who have injected drugs highlights concerns related to the spread of pathogens in detention centers as well as in communities, but also identifies an opportunity for intervention. Infectious disease screening is a clear option for identifying those who may be at risk for these conditions. The CDC recommends opt-out screening upon admission to jail36,37; however, surveys show only 7%–35% of facilities have adopted these practices.38 Rapid opt-out testing is feasible in jails,39,40 and this approach has been used effectively to identify new diagnoses at the time of admission,41 but more work is needed to determine how these practices can be implemented in small rural facilities in North Carolina.
The association between SUD, injection, and longer detention periods also introduces an engagement window for service initiation prior to release. Teaching harm reduction strategies and beginning treatment while incarcerated, for instance, could help connect people seeking care with needed services. This process could continue with a warm handoff to a community-based agency upon release, with follow-up testing and treatment to minimize unsafe injection practices.42
Continuity of care following release from jail is imperative, particularly for users of methamphetamine.32 This connection offers an opportunity to begin managing health conditions, but more research is needed to increase engagement and continuation following release from rural detention centers. There is potential to reduce substance use, criminal justice involvement, and dependence on jails as medical providers.
Although the results from the current study add to our understanding of relationships between SUD, injection, and jail readmission, there are limitations to note. Although the study was based on two detention centers categorized according to size with the majority of jails in the state, injection-related factors may vary in other counties. Replication studies are needed to further specify prevalence rates and how these relate to readmission across multiple counties.
Rural counties currently experience high rates of injection and the first step toward developing effective interventions involves understanding the factors associated with this condition. Detention centers in small communities represent primary points of contact for engaging people who inject drugs. Systematic rapid screening for injection-related diseases at the time of jail admission and connection to care at the time of release are vital steps toward community health and well-being.
Disclosure of interests
Data collection for this study was partially supported by C4 Recovery Foundation.