The outbreak of COVID-19 disproportionally affected Native Americans in the United States. Early data from the Centers for Disease Control and Prevention (CDC) showed that Indigenous populations were 3.5 times more likely to contract COVID-19 and 5.7 times more likely to be hospitalized for the virus.1 Increased testing and adherence to vaccination recommendations are two important strategies to manage COVID-19. These strategies further mitigate the impacts of the virus on marginalized communities. However, mounting evidence indicates that underserved communities, especially in the South, are less likely to actively participate in testing and vaccination.2 The underlying reasons explaining why underserved Indigenous communities experience relatively lower testing and immunization rates remain to be studied.
This study aims to examine Indigenous perceptions, attitudes, and behaviors about COVID-19 from a North Carolina Native American sample. North Carolina has the largest Native American population east of the Mississippi River and the eighth-largest Native American population in the United States, with more than half residing in rural, underserved counties.3 Indigenous populations in North Carolina report higher cases of COVID-19 compared to Whites and African Americans4 and lower adherence to vaccination.5 Moreover, there are limited available COVID-19 data from Native American populations because of the systemic erasure of Indigenous Peoples via inadequate Indigenous representation in data.6
This work is part of a larger ongoing project, Building Resilience And Vital Equity (BRAVE), focused on COVID-19 and Native Americans in North Carolina, funded by the National Institutes of Health. The project is a collaboration between the University of North Carolina, the Lumbee Tribe of North Carolina, and North Carolina Central University. The scope of the BRAVE project is to understand the Indigenous perceptions, attitudes, and behaviors about COVID-19 and design and implement culturally sensitive interventions to increase testing and vaccinations among Native American communities. This study is Phase I of the BRAVE project.
The goal of the Phase I study is to identify key factors that affect Native Americans’ testing and vaccination decisions and guide the study designs for a survey in Phase II and interventions in Phase III of the project. In Phase III, we use the data from Phases I and II to design two culturally sensitive interventions, Heath Education Campaign and Protect Your Elders Campaign, to address the barriers to testing and vaccination among Native American communities.
Indigenous Peoples living in the Southeast region of the United States comprise both federal and non-federally recognized tribes. The federal government’s denial of tribal recognition for some tribes, including the Lumbee, exacerbates the lack of fundamental trust of COVID-19 messaging from governmental authorities. Breaking the trust barrier by building positive relationships with Indigenous communities is crucial in this project. With the support of the largest Native American tribe in Southeastern North Carolina, the Lumbee Tribe, the team gained adequate trust in Indigenous communities and was privy to Indigenous attitudes regarding testing and vaccination for COVID-19, which further provided guidance toward culturally sensitive interventions.
Methods
This study serves as the critical first step in understanding Native Americans’ perceptions and concerns and identifying information, education, and communication needs for successful interventions. To serve the purpose of Phase I of BRAVE, we used a grounded theory approach to design interview questions. The interview questions were designed with the goal of allowing the respondents to tell their own stories, emphasizing concepts that resonate within the Native American community; our approach is to allow categories and domains/themes to emerge organically and not to prescribe through the use of literature and theory. To accomplish this goal, three Native American faculty investigators led the interview design and conducted the interviews. Also, the team engaged a community advisory board[1] throughout the process to seek feedback and input. The team conducted online interviews through Webex, a video conference tool, because physical proximity was limited due to the practice of social distancing. This study was approved by the Institutional Review Board of North Carolina Central University (NCCU).
Two researchers conducted 30-minute in-depth Webex interviews with 26 participants during March 2021 and April 2021. We used open-ended, semi-structured interview scripts to investigate participants’ overall perceptions of COVID-19. Interview questions incorporated a broad theme approach to examine varied needs for potential interventions.
The study participants were recruited from Pembroke, North Carolina. Pembroke and surrounding communities are nestled in rural countryside consisting of agricultural farming, longleaf pines, and swamplands. Indigenous Peoples living in the area include the Lumbee, Tuscarora, Cheraw, Cherokee, and Coharie, among others. Pembroke is home to the Lumbee Tribal Government and the University of North Carolina at Pembroke (UNCP), which is the only Native American University in North Carolina.
Indigenous Peoples of the area continually suffer from health, social, and economic disparities. Pembroke is located in Robeson County, a southeastern county of North Carolina whose population is 42% Native American.7 Compared with its neighboring counties and the state average, Robeson County has a high poverty rate, unemployment rate, and mortality rate8; Social Vulnerability Index9; COVID-19-positive rate10; and a significantly lower proportion of the population fully vaccinated for COVID-19.10 Robeson County reported its first clinically confirmed COVID-19 case on March 12, 2020, and as of March 2022, Robeson County had 43190 confirmed COVID-19 cases with 534 deaths.10
Analysis
All interview responses were audio-recorded digitally and transcribed verbatim. Researchers used a grounded theory approach to explore participants’ perceptions of COVID-19 and its related themes. Analysis of interview responses was reviewed independently by researchers along with data coding based on interview questions. First, researchers identified potentially useful concepts via open coding and then developed categories by integrating the relevant concepts and drawing connections between codes via axial coding.11 Further, researchers used SPSS to calculate inter-coder reliability. The kappa for overall categories across coders was acceptable (k = .91).12
Results
Characteristics of the Sample
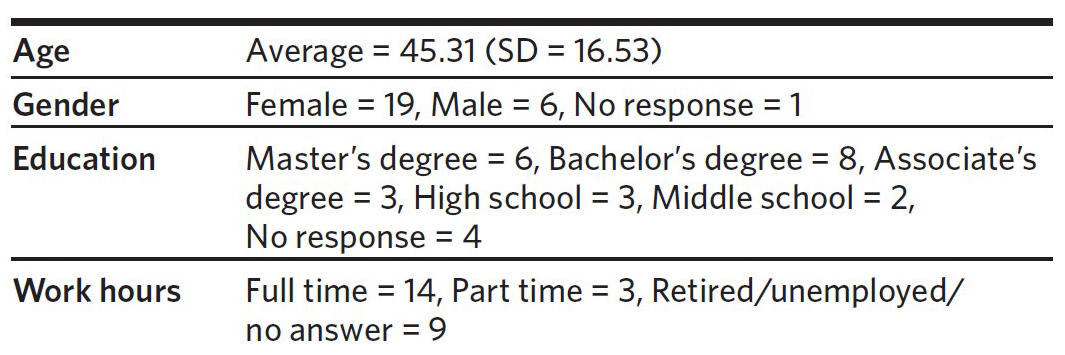
All participants were Native Americans living in Robeson County, North Carolina. The average age of participants was 45.31; most participants were women (female = 19, 73.08%; male = 6; no response = 1). More than half of participants had a bachelor’s degree or higher (master’s = 6, bachelor’s = 8, associate = 3, high school = 3, middle school = 2, no response = 4), with more than half of participants working full time (full time = 14, part time = 3, retired/unemployed/ no answer = 9) (Table 1).
General Knowledge about COVID-19
Researchers made an inquiry to understand general knowledge of, and life experience since, COVID-19. In response to the question about knowledge of COVID-19, most participants described COVID-19 as a highly contagious virus causing various symptoms (92%). While 27% responded that they experienced infection with COVID-19, 35% reported that Native Americans experienced more damage (e.g., death) from the COVID-19 virus than other ethnic groups. Upon inquiry about knowledge of the virus, one participant shared:
“I do know the symptoms. The symptoms include fever or chills, loss of taste or smell, muscle or body ache, headache, sore throat, nausea or vomiting, and diarrhea. And the symptoms can appear, I’m thinking within 10 days after it exposes to the virus.” (Participant #10)
Life Experiences Since COVID-19
Regarding the general life experience since COVID-19, the majority of participants reported the practice of social distancing (81%), while others reported increased time staying at home (65%). Participants also noted increased online education (31%) and having increased caution and fear of the disease (both 27%). Additionally, participants mentioned that they found new ways to interact and socialize with others (e.g., using Zoom conferencing) (23%). The same number of participants reported that the use of telecommuting had significantly increased since the quarantine/ stay-at-home orders (23%). Participants also shared suffering from depression and anxiety (23%). Deaths among family or close friends due to COVID-19 were reported by participants (19%).
“It’s changed my life because I missed going and visiting people, going to the grocery store. I don’t go unless I absolutely have to. You order your grocery … and pick it up because you don’t want to go in there shopping. I’m going to the doctor and you’re sitting in the car and then they call you when (it is) time to go in. Things are just so completely different.” (Participant #13)
Support Need
Researchers asked whether any support was needed due to COVID-19. Nearly half of the participants reported not needing any support (46%). On the other hand, some participants shared the need for mental health support (27%) or financial assistance (e.g., stimulus check, scholarship) (15%). Participants also responded to the question of what other people might need due to COVID-19. Participants emphasized the need for increased knowledge specific to COVID-19 and its vaccines (31%). Some also described social support (27%), nutritional needs (23%), and financial support (12%). Additional reported needs were transportation to and from testing and vaccination sites, internet access, and sanitizing supplies.
“We’re more fortunate than a lot of folks in terms of being able to continue to pay our bills and buy food. … we haven’t suffered … financially. It’s the social aspect that we’ve been closed off.” (Participant #5)
Information Sources and Trust
Researchers asked participants about informational sources used to learn about COVID-19 and their level of trust in the information. The majority of participants responded that they use television news and online news to learn about COVID-19 (81%). About half of the respondents mentioned using information from CDC or local health departments (42%). Some participants mentioned receiving information from family and friends (35%), health care providers (31%), or social networking services (31%). Regarding trust in information, half of the respondents shared confidence in the information they received (50%). Participants also complained about receiving confusing information (38%) and mentioned that they independently verified information (35%), while others only trusted specific informational sources (35%). More complaints include misinformation about COVID-19 (23%), lack of trust in vaccines due to political reasons (23%), and no trust in social media (19%).
“.. just being Native, … I kind of have less trust in what the government says or does or provides, especially in terms of medicine. … I think that’s been like a learned behavior for the country, so I wouldn’t say I trust, … but once I dig into it a little bit, I believe what I’m researching.” (Participant #6)
“Our grandmother on her death certificate, she had COVID along with four other things. … we know she tested positive three weeks before she died.. but still (some) family members were saying ‘they just put that on their death certificate so the hospital can get a bonus.’ … it’s even more fuel for the conspiracy fire. They’re just adding COVID on it and running up the numbers to scare us.” (Participant #9)
Efficient Way to Communicate
Researchers inquired about the most efficient way to communicate with Native Americans. Participants recommended local health department outreach (35%) and communication through the tribal office or community church (31%). Recommendations further included the use of social media (27%), Lumbee tribal newsletter (19%), trusted Indigenous community members (15%), and distribution of flyers to heavily visited locales (e.g., grocery stores) (12%).
“(Health department) has brought the shots into the community and given them at one of our facilities twice now, and if that continues, that is extremely helpful. When they do that, they do take the time to talk to people and discuss about COVID.” (Participant #8)
Vaccination and Testing
Researchers asked several questions to learn participants’ perceptions of vaccination and testing. First, in response to perception of testing, 16 participants reported being tested (62%), and more than half of the participants showed a positive perception (58%) of testing, while others showed a negative perception (23%). Participants also mentioned that people they know expressed more negative perceptions (38%) than positive perceptions (15%) of testing. Complaints about testing included people who do not consider the virus serious (35%) and question the accuracy of test results, testing reliability, and validity (23%). Some participants also pointed out political reasons to avoid testing (23%) and shared concerns about the stigma of being tested (19%). Other complaints included the price of tests, limited access, and different testing methods (each 15%).
“The rapid test they have right now is just so unreliable. I think it is a lot less reliable than what they’re even reporting because you can take the test 1 minute, turn around, take it again and get a totally different marker.” (Participant #11)
In response to perceptions of vaccination, 11 participants said that they are vaccinated (42%), which is very close to the percentage of Native American respondents who reported vaccination hesitancy (40%) in the American COVID-19 Vaccine Poll,13 and five participants mentioned they plan to receive vaccination (19%). About half of the participants showed positive perceptions of vaccination (46%), but at the same time, there were some negative perceptions and concerns (31%). Similar to the perceptions of testing, participants mentioned that they perceive others as having more negative perceptions (62%) than positive perceptions (27%) of vaccination. Researchers also inquired about the reasoning behind these different perceptions. Positive perceptions of vaccination came from the feeling of safety and comfort after vaccination (15%). Minor opinions suggested that the vaccine would decrease the severity of the virus and death rates. On the other hand, there were several reasons for the negative perceptions of vaccination. The biggest concern was the side effects of the vaccine (42%). Some participants were concerned about the safety of the vaccine because it was authorized for emergency use (31%). Other participants also shared a lack of trust in the vaccine (31%), and a few participants mentioned political reasons (15%). Further still, some participants expressed overconfidence in their health, feeling the lack of need to be vaccinated (12%), and a few participants shared concerns about the vaccine’s effectiveness in protecting against variants (12%). Collected opinions included questions about the duration of effectiveness, complaints about limited access to the vaccine, vaccine pricing, and lack of clarity regarding whether previous COVID-19 infection requires additional vaccination.
" … a lot of them talk about not wanting to get the vaccine because they think that they’re either going to get COVID from the vaccine, or it’s going to have negative side effects. … Some people are just like, ‘I’m not going to get the shot because there’s no point.’ I don’t think they’re fully educated yet about how beneficial the vaccine will be. I’m hoping that … (they will) know more information about the effectiveness of the vaccine and why it’s important to get it. So that way, we can stop the spread of it everywhere, but especially in our tribal community, because we’ve lost a lot of people due to COVID." (Participant #1).
Masking, Hand Sanitizing, and Social Distancing
Researchers inquired about perceptions of wearing masks, using hand sanitizers, washing hands, and social distancing. A significant number of participants responded that they wear a mask (73%) even if they don’t like it (31%), and two participants responded that they don’t wear a mask (8%). Most participants supported hand washing (96%) and social distancing (92%).
“I have 5 or 6 classmates passed. I have friends that died … shouldn’t be dead … because they would not wear a mask. I mean one of them that would tease my husband every time he saw him. He is in (a) grave now and died from COVID.” (Participant #5)
Protecting Elders
Researchers asked participants’ opinions about how to protect their elders from COVID-19. A significant number of participants mentioned that close family members should be more cautious (69%) and need more education on COVID-19, masks, social distancing, and hand sanitizing (50%). Some participants mentioned increasing social support through outreach programs (42%) and assisting elders in receiving a vaccination (27%). Some participants also mentioned a community delivery service (e.g., grocery) (27%) and increasing the safety of social gatherings through web conferences (15%). Opinions further included phone calls to elders and providing more supplies, such as hand sanitizers and tests.
“They (elders) need to stay away from young people because a friend of my family’s, she died because her grandchildren … lived with her, and they … brought it home to her. She had not been going out anywhere, had been wearing (a) mask and doing everything, but it still came in the house.” (Participant #11)
Discussion
This study sought to explore factors associated with Native Americans’ testing and vaccination decisions based on perceptions, attitudes, and behaviors related to COVID-19. Overall, COVID-19 was a widely known disease that was understood generally in terms of symptoms. Although wearing a mask, hand sanitizing, and social distancing had very high support, perceptions of testing and vaccination decisions were mixed. The overall impression was a constant need for information accuracy, need for knowledge transference, and lack of trust.
While 81% of participants use television news and online news as the main sources to learn about COVID-19, only 42% of respondents mentioned using information from CDC or local health departments. Existing studies show that participants who have more trust in medicine learn information from health care workers and health officials, whereas those who have less trust in medicine are more likely to use information collected from social and online media.14,15 Native Americans have long experienced governmental distrust due to issues including genocide, family separation, culture termination, and forced assimilation practices. The transference of elder wisdom cultures has led youth to suffer drastically from the impacts of mandatory assimilation. Consequently, a reluctance to rely upon messages from the government is common.
Participants shared concerns about information inaccuracy and insufficient information. About half of the participants (42%) emphasized that they need more specific information about COVID-19, testing, and vaccination to increase community awareness and knowledge. This finding aligns with recent literature on vaccine hesitancy in minoritized communities.16–20 Current mistrust could be driven by historical injustices, distrust of the political administration, and a lack of trust in the health care community.21–23 Native Americans have faced health and health care disparities from social and economic factors, underlying health conditions, and lack of health care access.24 Existing literature on pro-vaccine intervention also suggests evidence-based practices, such as providing education to increase awareness of the safety and efficacy of the vaccine and working with community stakeholders to increase access and rebuild trust in prior interventions.25–28
The following are the questions participants have about COVID-19 that may help build up future interventions.
COVID-19 general information: How do people get infected? How does the virus spread, and why is wearing a mask important? Who has a higher risk? How long does it take to show symptoms? How long can one person infect others? How does asymptomatic infection work? If a person had COVID, can he/she get COVID again? How far apart? What are the different types of COVID variants, and what are the symptoms of variants?
COVID-19 testing: Who needs to get tested? What are the example symptoms to get tested? How often does someone need to get tested? How does someone make an appointment for testing? What are the different types of testing methods? Where can you get free testing? Is there any accessibility support? How fast can you get the testing result? How accurate is the testing result?
COVID-19 vaccination: Who needs vaccination? Do people who got COVID-19 still need shots? What health conditions mean a person can (or cannot) get the vaccination? What is mRNA, and how safe is it? What are the benefits of vaccination? Is the vaccine effective on variants? What are the side effects and their severity, including long-term side effects? Where can I get the vaccine, and what is the price? How can I make an appointment for vaccination? Is there any accessibility support?
Limitations
This study’s findings should be generalized with some caution. This study included a small sample size, which makes it difficult to include a diversity of demographic backgrounds (e.g., gender, education level, tribe, etc.). Additionally, although participants could join by phone, the online format of the interviews may still have prevented people from participating due to being unfamiliar with the online meeting format and limited internet access in some Indigenous communities. Thus, future studies should develop an active approach to including more diverse participants. To our knowledge, this is the first study that uses a qualitative approach to understand COVID-19 perception among Native Americans in Robeson County, North Carolina.
Conclusion
The study has identified information that revealed insufficiency related to COVID-19 knowledge transference and the need to increase knowledge about COVID-19 among Native Americans in North Carolina. Findings confirmed that the lack of reliable information and lack of trust plays a significant role in intensifying the impact of the COVID-19 virus on the Indigenous marginalized community. Researchers further conclude that interventions require inclusionary investments in public health information at federal, state, and community levels. These investments are warranted for addressing the structural insufficiencies in providing more specific information to Native Americans on health-related matters. The Indigenous underserved communities deserve more effective infrastructure, such as a community dashboard that communicates data on COVID-19 testing and vaccination serving the Native American community in particular as a trusted, community-driven resource providing the necessary information and support to combat future public health emergencies.
Acknowledgments
The authors gratefully acknowledge the support for BRAVE from the NIMHD grants 3R01MD012767-04S1.
Disclosure of interests
No interests were disclosed.
The community advisory board consists of community members with diverse backgrounds, including business, health, town government, tribe government, and ministry.