“America’s veterans are the best of us…we have a sacred obligation…to care for them and their families when they come home. This is especially for veterans suffering from the visible and invisible wounds of war…that come from hazardous exposures, which have gone unaddressed for too long” – President Joseph R. Biden, 2022.1
Introduction
North Carolina boasts the fourth-largest population of military Service Members in the United States at over 100,000, and approximately 700,000 Veterans reside in the state.2–4 For context, as of 2021, roughly 16.5 million Veterans and 24 million military family members live in the United States. The Department of Veterans Affairs (VA) provides care to about 9 million Veterans; less than half of those seek care within VA treatment centers.5,6 Access to care for Veterans in VA medical centers is limited by the extent of their service-connected conditions. Most Veterans receive care in the community. After the passage of the Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018, there were 12 million referrals to civilian sites from 2019 to 2021.7 As millions of Veterans and Service Members seek care in the community, it is important to understand the needs of this vulnerable population and their occupational exposures. Nurses and other health providers report feeling underprepared to recognize military status or to care for military-service-related health problems.8 Poor cultural competence and inadequate preparedness to recognize and treat service-related/suspected medical complications are formidable for any civilian provider.9
During military service, most Service Members will have some exposure to hazardous substances, as the business of the military engages with chemical, biological, radiological, nuclear, and explosive materials at home and when deployed. Most post-911 Veterans who were stationed in Iraq and Afghanistan were exposed to hazardous burn pits.10 Exposures to toxins unfortunately also occurred prior to 911 at bases in the United States. In North Carolina, Service Members and their families who were stationed at either Marine Corps Air Station New River or Marine Corps Base Camp Lejeune from August 1, 1953, through December 31, 1987, were exposed to contaminated drinking water containing benzenes and other chemical solvents.11
Conditions Related to Toxic Exposures
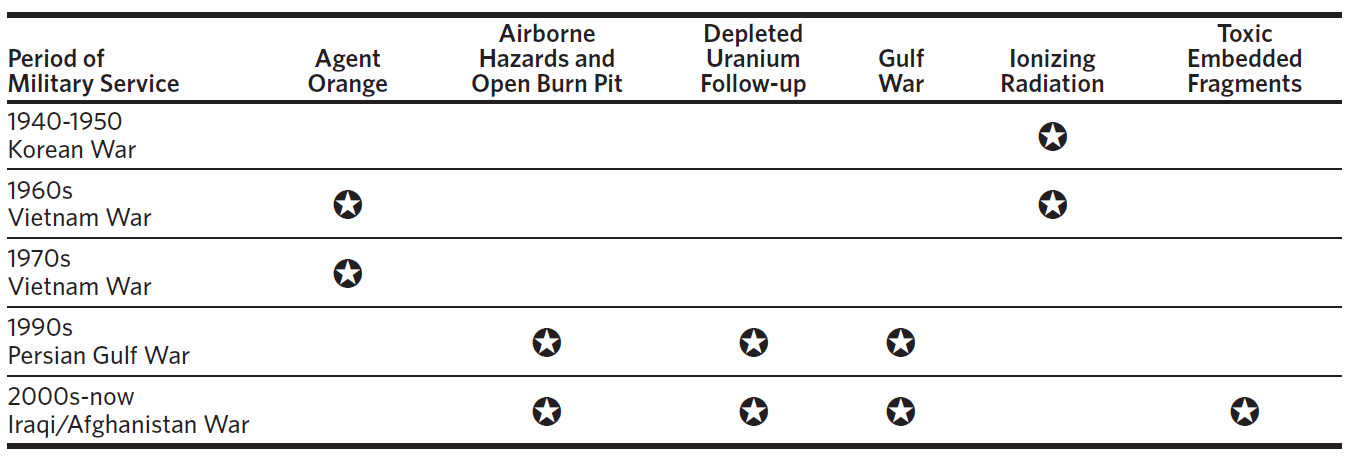
Toxic exposure is unique to each Service Member and Veteran, as military experiences vary by generation and branch of service based on military specialty/job requirements and occupational/environmental elements related to geographical areas of conflict. Exposures to chemical weapons, asbestos, nuclear radiation, and environmental hazards predispose Service Members, Veterans, and their families to medical conditions highlighted within existing legislation, VA registries, and VA/Defense Health Agency (DHA) policies. Table 1 provides a depiction of service-connected exposures based on era of service created by the VA to guide clinicians and Veterans to the environmental health registry that is most appropriate in order to establish evaluation and treatment in VA facilities.
Illness, injury, or diseases that may not have been apparent at separation from the military may worsen over time, and this is especially true with toxic exposure complications. Identification and recognition of medical complications related to toxic exposure have recently heightened after years of perceived failed promises to Veterans and their family members. The Sergeant First Class Heath Robinson Honoring Our Promise to Address Comprehensive Toxics Act (PACT Act) was designed to expedite Veterans’ diagnosis of service-connected conditions related to toxic exposures through a presumption of illness based on time/location during active service.12 Eight medical conditions related to these exposures—including leukemia; aplastic anemia; cancers of the bladder, kidney, or liver; multiple myeloma; non-Hodgkin’s lymphoma; and Parkinson’s disease—are eligible for cost-free care in the community under the MISSION Act based on conditions that are covered in the PACT Act.
Ratification of the PACT Act dramatically improved access to care and recognition of illness from suspected toxic exposures while challenging the VA health care system to prepare for a mass increase in patient volume and complexity. There were over 3.6 million toxic exposure screenings and over 627,000 PACT Act claims submitted within the first year of enactment.13 On July 14, 2023, the Department of Veterans Affairs achieved a significant milestone by successfully completing toxic exposure screenings for 4 million Veterans as part of PACT Act implementation. Approximately 42% of Veterans screened reported at least one potential exposure during their service, initiating important discussions between Veterans and their health care providers.13 The impact of the PACT Act on civilian treatment facilities has yet to unfold, but there is likely to be an increase in referrals and more Veterans will likely use it to access treatment for newly diagnosed service-connected complications related to toxic exposures. Veterans who are diagnosed with service-connected conditions will now have continued access to care in the community via the MISSION Act and increased benefits by newly defined presumptive conditions in the PACT Act.
Cultural Competence for Providers
Health care providers’ lack of cultural competence regarding military service is a barrier to Veteran care, and a minority of non-VA health care providers regularly screen for past military experience.14 Understanding military status and culture is an identified shortcoming that degrades military-informed care (health practices based on the military background) and thus, overall Veteran and Service Member health and well-being.9,14 Failure to identify military status leads to incomplete medical screenings and identification of toxic exposure for Veterans.14,15 Research supports poor provider knowledge regarding military environmental/toxic exposure from inadequate training and lack of access to clinical references.16 To address these gaps, Veteran-centric competencies and knowledge/teaching strategies should be developed to facilitate the application of Veteran-centric care.9,14,16 The infusion of military/Veteran concepts into undergraduate medical and nursing programs would enhance cultural understanding, disease screening, and military cultural fluency and have a positive impact on Veteran-centric care outcomes.9,17,18 Improving patient-provider interactions through vetted communication tactics and established clinical tools would likely improve overall patient-provider satisfaction and clinical outcomes and bolster military/Veteran cultural fluency in the medical community.14,16
The first step for providers is to identify patients who have served in the military. In 2011, First Lady Michelle Obama and Second Lady Dr. Jill Biden launched Joining Forces, an initiative that worked with the public and private sector to ensure that Service Members, Veterans, and their families had access to wellness, education, and employment opportunities.19 The American Academy of Nursing (AAN) Military & Veteran Health Expert Panel and the Presidential Joining Forces initiative launched the “Have You Ever Served?” campaign in 2015 to guide providers through general intake questions regarding Veteran/military status.20 Similarly, Military One Source (MOS) initiated the “Ask the Question” campaign to better connect Service Members, Veterans, and their families with state and federal resources by recommending providers ask, “Have you or you a family member served in the military?” on intake forms.21 Asking these questions is not always easy, as there may be some concern about what to ask next or how a Veteran may respond. However, it is essential for Veterans—particularly those with toxic exposures—to receive the appropriate care and benefits.
Resources for Providers
Several other educational resources for health care providers are available to support clinical practice. The VA, VA-War Related Illness and Injury Study Center (WRIISC), Department of Defense (DOD), Defense Health Agency (DHA), Centers for Disease Control and Prevention (CDC), Office of Personnel Management (OPM), American Academy of Colleges of Nursing (AACN), and several other agencies offer civilian providers/clinician courses free of charge to bolster Veteran cultural competence. The VA and DOD/DHA courses have several modules, including culture and concepts specific to military/Veteran health, such as post-traumatic stress disorder (PTSD), military sexual trauma (MST), suicide, and introduction to exposure registries. The VA has partnered with the American College of Preventive Medicine (ACPM) to offer Level I Certification in Military Environmental Exposures. The certification is for all providers and will equip each participant with the skills and knowledge needed to effectively identify, treat, and manage the effects of environmental exposures for this population. The VA also offers a reference called the Military Health History pocket card for health professionals that provides a comprehensive history-taking/interview approach to addressing Veterans’ medical concerns.22 Additionally, the VA created a phone application called VA Mobile-Exposure Ed, which clinicians can use to reference exposures based on location, date, and conflict.23 Finally, to visualize the impact of the PACT Act on health care, the VA has created a VA PACT ACT Performance Dashboard, which gives biweekly updates regarding the total number of screenings completed, clinical outreach efforts, and geographical analysis at national and state levels.13
Veterans can self-enroll into one of the six registries for service-connected complications: Agent Orange (AO), Airborne Hazards and Open Burn Pit, Depleted Uranium Follow-up, Gulf War, Ionizing Radiation, and Toxic Embedded Fragments. Table 1 displays current VA registries related to decades of service or military conflict. Enrolling in these registries alerts Veterans to possible medical conditions that may be related to environmental hazardous exposure that they experienced during military service.
A Veteran Exposure Assessment Screening and Evaluation (VET-EASE) toolkit was developed as a means for providers to address the identified needs of Veterans suffering from conditions related to toxic exposures. This toolkit is in the initial proof-of-concept phase as a Veteran-centric competency for clinical providers addressing occupational and environmental hazardous exposures. Initial response is overwhelmingly positive. The VET-EASE toolkit is intended for primary care provider use when interacting with Veterans who present with medical concerns perceived to be related to toxic exposure. It was developed as part of an initiative of the AAN Military/Veteran Expert Panel to develop Veteran-centric primary competencies, and the panel served as an Advisory Board as the toolkit was piloted with 30 providers in VA Primary Care centers. The VET-EASE toolkit is an example of evidence-based/infused clinical decision-making tools based on Veteran-centric competencies and can serve as a model for future toolkits (Table 2).
Conclusion
The influence of the PACT Act on health care for Veterans, Service Members, and their families is transformational. However, there is a need for more efforts to foster civilian clinician training regarding Veteran-centric competencies. Veterans need access to health care at national and state levels as most seek care through civilian health care organizations. As the PACT Act has improved access to care and visibility of medical conditions from suspected toxic exposures, academia and research need to evolve to support the clinical knowledge needs of those caring for members who, in defense of our nation, have been exposed to these environmental hazards.
Disclosure of interests
No interests were disclosed.