Introduction
Despite the steady decline in cancer incidence, cancer remains the second leading cause of death in the United States.1 The disproportionate cancer burden faced by some communities has led to a greater emphasis on identifying practical ways to reduce cancer risk and improve access to care.2,3 In 2022, as part of the Moonshot 2.0 announcement, President Biden charged everyone in the nation to identify ways to collaborate with each other to end cancer as we know it, with a more specific task of reducing cancer mortality rates by 50% over the next 25 years.4 To provide a framework in support of this goal, the Director of the National Cancer Institute (NCI) released a National Cancer Plan in April 2023, designed to guide the nation’s collective efforts to reduce overall cancer burden.5 The Cancer Plan outlines eight goals, including improving cancer prevention, early detection, and effective therapies; but one of the most challenging goals outlined is that of eliminating inequities in cancer care.
Disparities in US cancer incidence and outcomes have been well documented for a variety of communities, including populations defined by race/ethnicity, geography, age, and sexual orientation/gender identity, to name a few.6–8 While strategies and frameworks for improving cancer equity have been published,9–11 the design and implementation of sustainable programs to mitigate cancer disparities at the institutional level is often nuanced and requires input from the communities at greatest risk for poor outcomes. Herein, we describe an innovative Population Health Navigation Program that was derived from a community-engaged approach to improving cancer care for marginalized communities in North Carolina.
Background
The Atrium Health Wake Forest Baptist Comprehensive Cancer Center (AHWFBCCC) is an NCI-designated comprehensive cancer center committed to providing access to quality care for all patients regardless of where they live or their background. In 2014, the Office of Cancer Health Equity (OCHE) was developed to champion cancer health equity and community engagement activities. Its mission is to advance community engagement, clinical care, and research focused on improving outcomes for everyone in our communities, with special emphasis on those with worse cancer outcomes and greater barriers to accessing cancer care.
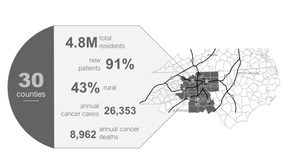
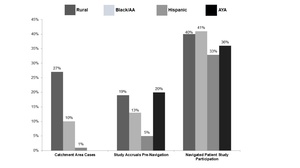
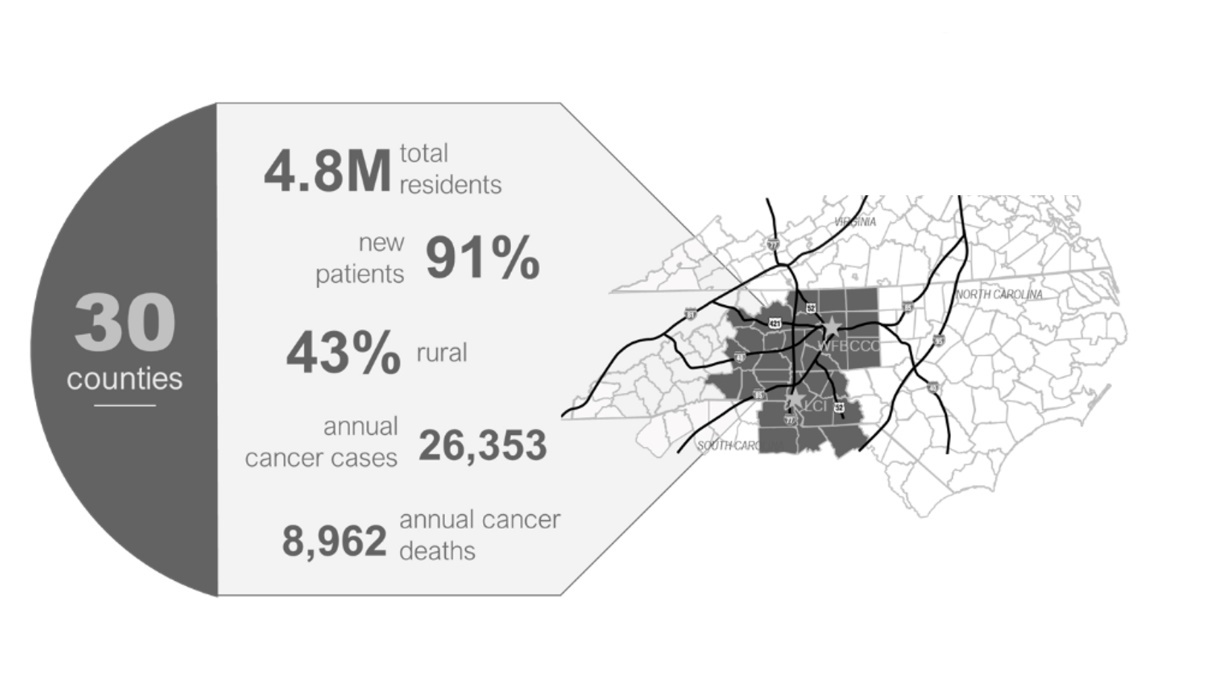
AHWFBCCC’s primary impact area is a 30-county region in Western North Carolina and Northwest South Carolina (Figure 1) with over 26,000 new cancer cases per year. This geographic area includes 4.8 million residents, about one-third racial/ethnic minority, and 43% of the counties are designated as rural. The region is also characterized by high rates of poverty and limited access to health care, which, in addition to high rates of tobacco use when combined with a strong presence in tobacco production and cigarette manufacturing, contribute to elevated incidence of lung, head and neck, and bladder cancers. There are also higher incidences and mortality rates for rural versus urban communities within the region, as well as higher incidence and mortality rates among Black patients when compared to their White counterparts.
To address cancer disparities in the area, OCHE leads multiple community initiatives focused on underserved populations. In 2015, OCHE collaborated with community members and community-based organizations to launch the Population Health Navigation Program with an initial emphasis on providing services to the growing Hispanic population in the region. The program was designed to reduce barriers to care experienced by patients from traditionally underserved communities during cancer treatment. This innovative program hires professional non-clinical navigators to provide support services for health-related social needs in a culturally and linguistically concordant manner along the entire continuum of care, beginning with community outreach and engagement.
Program Development
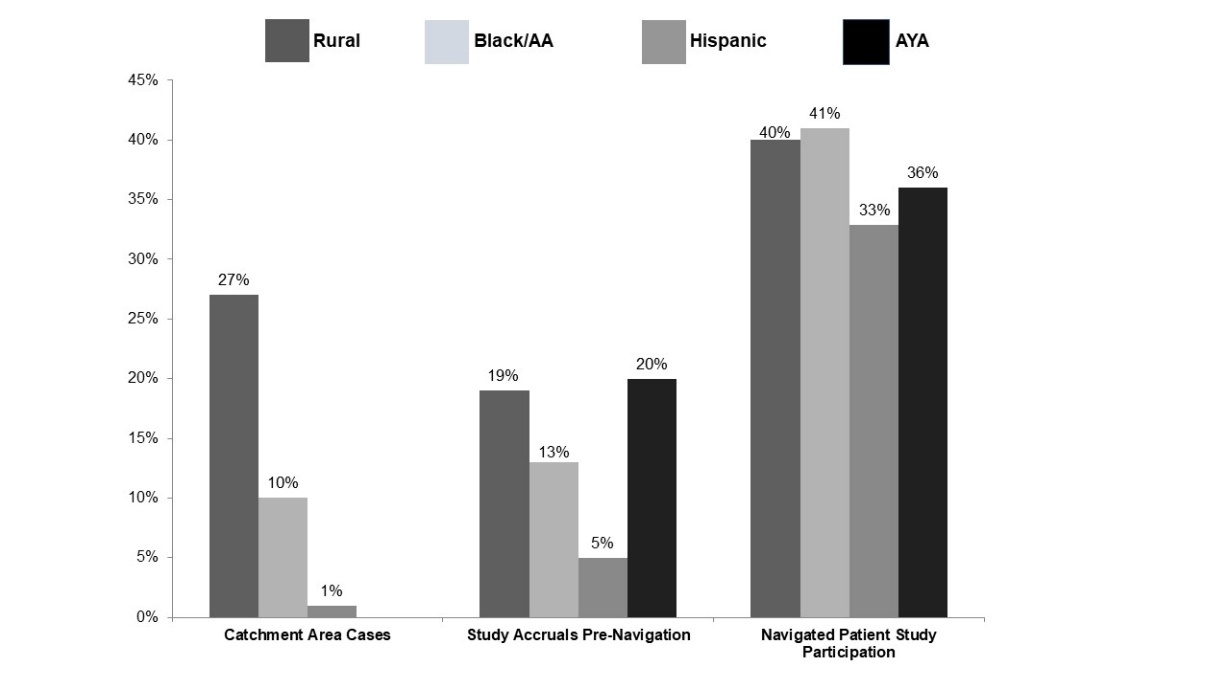
The Population Health Navigation Program was initially partially financed by external funding sources. A small grant from a community partner enabled OCHE to hire a bilingual, bicultural navigator focused on improving cancer knowledge, expanding access to screening, and reducing barriers to health care access for the Hispanic population. The navigator started engaging the Hispanic community, becoming a trusted partner well before patients and families have a cancer experience. Now, if a cancer diagnosis is made, the navigator frequently already has a relationship with community members, enabling a smoother transition into cancer care. A variety of metrics were used to evaluate programmatic success, including the number of community members served and patient satisfaction. However, to ensure sustainability of this nascent program beyond the grant period, it was vital to show benefit to the institution. Patients showed a 15% increase in knowledge about cancer and clinical trials and the percent of navigated Hispanic patients who participated in clinical trials was as high as 39%.12
Recognizing the diversity of our catchment area and understanding how cancer impacts specific populations, OCHE worked with community partners to tailor the Population Health Navigation (PHN) Program to other underserved populations. In 2018, grant funding was obtained to expand the program to provide concordant care to Black patients and those living in rural communities in North Carolina. OCHE prioritized a rural patient navigator to address the unique needs of our geographic region. As a gateway city, Winston-Salem connects the mountainous Appalachian and predominantly homogenous rural communities with the more urban northwest Piedmont region of North Carolina. Individuals living in rural counties in the United States have a 17% higher death rate from all cancers combined compared to patients in urban areas; rural residents tend to have lower income and be older, less educated, and less likely to have health insurance.13 Transportation was found to be the greatest barrier to cancer care for all populations in our impact area, but patients living in rural counties travel on average 171 miles round trip to receive cancer care at AHWFBCCC.
In contrast, Winston-Salem is home to a diverse population of over a quarter of a million people who identify as Black/African American (34.2%), Hispanic or Latino (15.1%), or as two or more races (5%), making it a majority-minority city. To address the disparate social and health needs of the Black community and higher rates of medical mistrust of our institution due to eugenics and past discrimination within the health care field, a navigator role focused on the Black community was established. Evaluation of the PHN program following the addition of the first two navigators showed continued success with high rates of patient satisfaction, robust community engagement, and as much as a 50% increase over baseline accrual into research studies.14
Program Implementation
Connecting Patients to Navigation
PHNs are unique in that they help patients throughout the entire cancer continuum. Each navigator is involved in community outreach and engagement for their respective populations so that they are working with and building relationships in the communities they serve before a cancer diagnosis. However, once a patient from any of the navigated groups seeks care at AHWFBCCC, they are connected to their culturally and linguistically concordant navigator prior to their first visit and are navigated from the time of initial diagnosis through to survivorship or end-of-life care.
At the beginning of the program, eligible patients were identified via an internally designed bio-informatic algorithm that searched the electronic medical record (EMR) daily to identify individuals from the respective communities who had new appointments at the cancer center within the coming two weeks. Navigators would then filter through their respective lists of patients and confirm eligibility prior to reaching out to conduct an initial assessment. Race/ethnicity, age, and ZIP code were verified using the EMR. The rural navigator applied the USDA’s Rural Urban Commuting Codes (RUCA) and the Rural Urban Continuum Codes (RUCC) to determine rurality, easily accessible through the Rural Health Information Hub’s “AmIRural” tool. Codes 1–4 designate an urban area and codes 4–10 designate a non-urban or rural area.15
Although the bio-informatic algorithm is still occasionally utilized, due to the rapid growth of the program and institutional buy-in from leadership and team members across the cancer center patients now are typically identified through referrals by the multidisciplinary care team (i.e., physicians, advanced practice providers, ambulatory nurses, nurse navigators, front desk personnel, etc.). Navigators also rotate through tumor boards monthly and proactively reach out to patients who are classified as having health-related social needs and identify with the populations served. Referrals are made through the EMR or over the phone, email, or pager. Navigators can communicate directly with clinical staff through telephone notes and staff messages.
Documentation/Tracking
The navigators document interactions in the EMR and utilize the HealthyPlanet Module to track activities and manage case load. A HealthyPlanet flowsheet was developed to document assessments, barriers, health-related social needs, and interventions throughout the patient’s active treatment. A flowsheet is entered for each interaction with a navigator, indicating who the interaction was with (member of health care team, caregiver, patient), how they communicated (phone, email, in person), and the length of the interaction. For reporting purposes, reports generated in the EMR are utilized to track case load, barriers, and interventions.
Also documented in the EMR is the intensity of navigation a patient is expected to need. The use of acuity scales to assess cancer patient needs when undergoing treatment is gaining recognition as a way to optimize case loads.16 We developed a novel approach to an acuity scale to systematically allocate navigation services. The instrument is designed to pre-identify the level of navigation services required in order to inform stratified care based on patient characteristics and barriers. The level of navigational services (intensity) is based on acuity scores determined by patient characteristics and barriers to care.
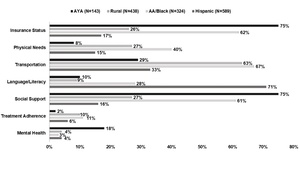
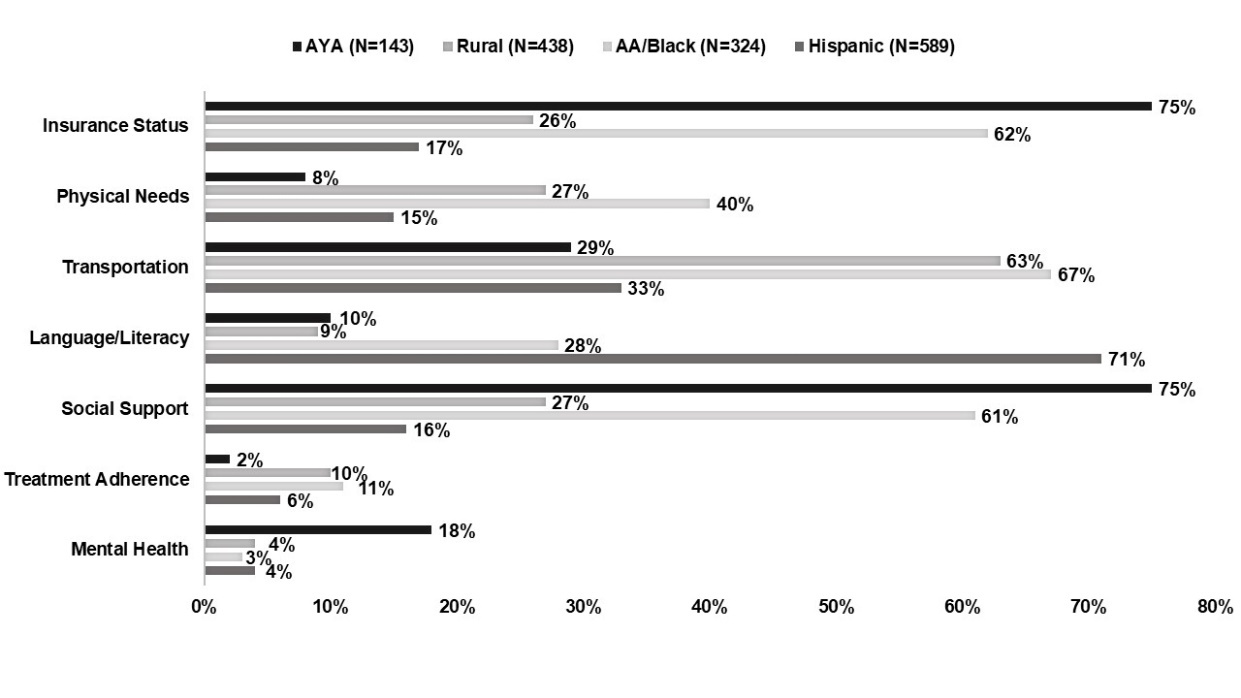
Patient characteristics include disease site, cancer phase, age, and treatment factors, among others. Patient barriers include drivers of potential impact on care, such as insurance status, language/literacy, social supports, transportation, and others (Figure 2). Each individual characteristic or barrier is assigned a score of 0, 1, 2, or 3, with intensity level increasing exponentially. These are totaled and assigned a score ranging from 0 to 20+. The intersecting scores are combined to generate four intensity levels: no, low, medium, and high navigation. Navigators then follow guidelines of minimum interactions per month with each patient; for example, if a patient is “high” acuity, the guidelines require navigators to interact with the patient at least one time per week. Acuity can change as the patient’s journey through active treatment continues. Ideally, the intensity scale is administered at first interaction and re-administered at pre-set intervals throughout the patient’s active treatment, or with any major change in patient status or social situation.
Role of Navigation in Research
Patient navigators are currently underutilized but well-suited to providing education, financial assistance, and decision-support services around participation in clinical trials.17,18 They can help patients weigh their unique concerns around—and remove potential barriers to—receiving care through standard treatment versus replacing or accompanying it with a cancer clinical trial. To capitalize on the expertise of the navigators, OCHE developed a short educational curriculum and designed the patient intake process in such a manner that they provide tailored education to each patient on the role of research in cancer care, often before the first clinical encounter. Patients are educated about the different types of trials and why cancer research matters—particularly for underserved populations—and can address historical injustices while emphasizing current patient protections.
While navigators do not represent a specific study or enroll patients in or consent them for treatment trials, they advocate for informed decision-making and empower patients to ask pertinent questions about the cancer treatment, including asking if there might be a research study available to them. Whether patients participate in a clinical trial as part of their initial treatment or years later in survivorship, the concept and conversations around cancer research and clinical trials are normalized to increase likelihood of participating.
Sustainability/Funding
OCHE was fortunate to receive grant funding from community-based organizations and the NCI to support communities and patients from three of the most underserved populations seeking care at AHWFBCCC. Following the success of the Hispanic, Black, and rural navigators, in 2022 OCHE sought funding to add a navigator to address barriers in adolescent and young adult (AYA) patients (age 15–39), the most underserved age group in cancer care.19,20
Due to its demonstrated impact, the Population Health Navigation Program has garnered tremendous support from cancer care providers and institutional leaders and is now fully supported by the institution.
Measuring Impact
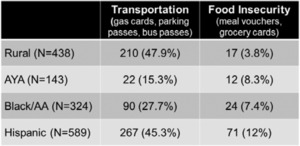
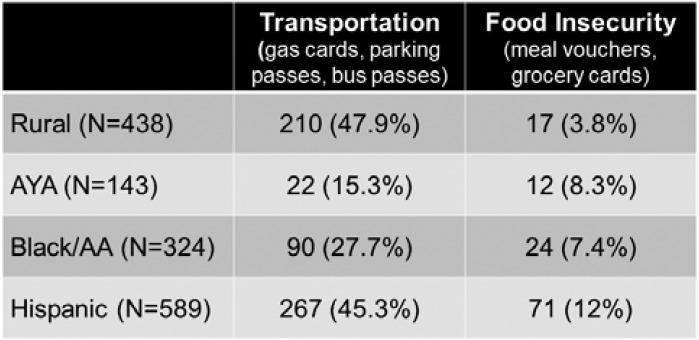
Since the program’s inception, 1,494 patients have been navigated. Barriers to cancer care include insurance status, physical needs (food, clothing, housing), transportation, language/literacy (preferred language, health literacy), social support, and missed appointments, though these vary by population (Figure 2). Common barriers for AYA patients include insurance status (75%) and social support (75%). Rural (63%), Hispanic (33%), and Black patients (67%) struggle with transportation. The most common barrier for Hispanic patients is language/literacy (71%), whereas notable barriers for Black patients include insurance status (62%) and social support (61%). The navigators work to address these barriers through referrals to internal and external partners. They are also able to assist patients with direct support through gas cards, bus passes, parking passes, meal vouchers, and grocery cards, as seen in Table 1.
As a result of intentional educational programming, participation of navigated patients in clinical research is substantially higher since implementation of the Population Health Navigation Program (Figure 3).
Future Directions
The cancer center has expanded due to a recent merger, and inclusion of the Charlotte campus provides an opportunity to extend and adapt the PHN Program to impact a much greater number of patients. Additionally, we continually assess our impact area to identify other populations (e.g., people with disabilities, LGBTQ+) with unique experiences that may benefit from Population Health Navigation to improve cancer equity.
Acknowledgments
The OCHE Population Health Navigation Program was initiated with funding from Winston Salem Foundation (Hispanic population); the NCI - grant P30CA012197-43S2 (rural population), the V Foundation (Black/African American population), and Teen Cancer America (AYA population).
Disclosure of interests
No interests were disclosed.