Introduction
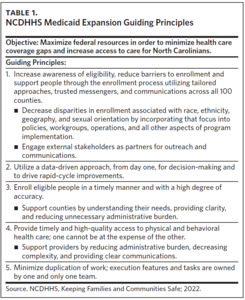
On December 1, 2023, North Carolina became the 41st state (including Washington, D.C.) to expand Medicaid under the Affordable Care Act. The North Carolina Department of Health and Human Services (NCDHHS) expects Medicaid expansion to provide health coverage for over 600,000 North Carolinians. In preparation for the launch of expansion and building on lessons learned in the COVID-19 pandemic response, NCDHHS established guiding principles and pledged to involve trusted community partners for a continuous flow of information, ideas, and real-time feedback on our approach. Our overarching goals to get people covered, get people care, and collaborate with our partners play a key role in how we plan to evaluate our success. Our evaluation plan for Medicaid expansion in North Carolina relies on our guiding principle of using a data-driven approach to decision-making and driving rapid cycles of improvement (Table 1).
Using Quantitative Data
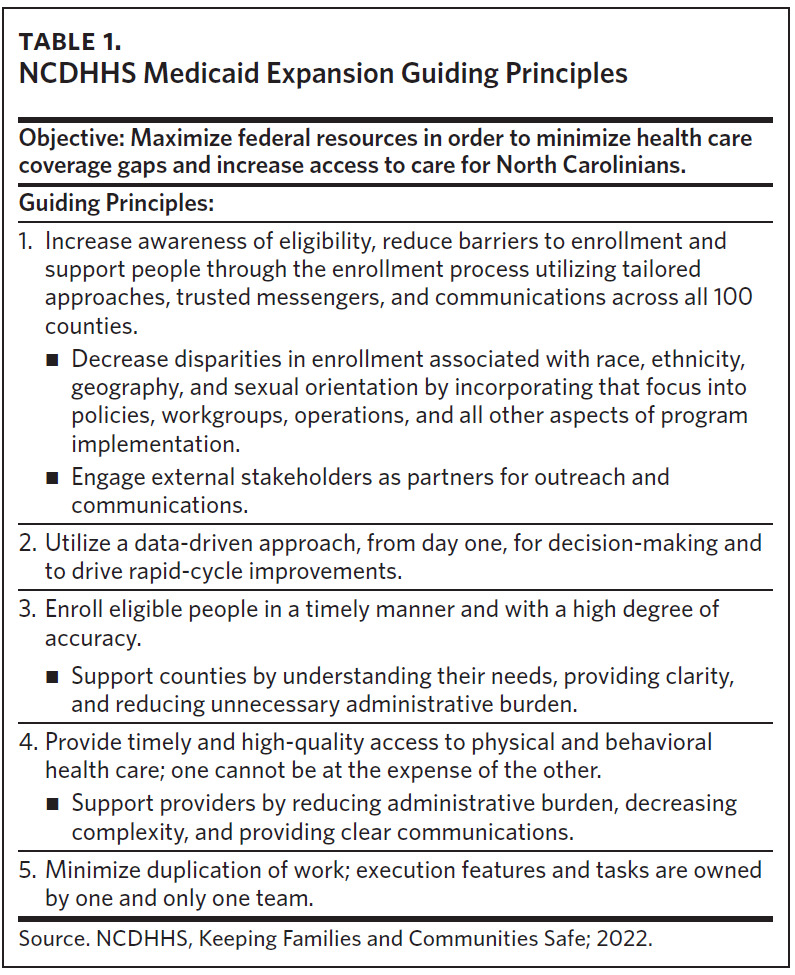
Timely access to meaningful data is a best practice from other expansion states. One way we plan to use quantitative data for evaluation is through our public-facing Medicaid expansion dashboard. In an effort to capture requirements and feedback from a wide range of perspectives, the Division of Health Benefits Business Information and Analytics team solicited feedback on prototypes of this dashboard from NCDHHS leadership and various external partners throughout the development process. The dashboard will track monthly enrollment counts across seven sets of demographic strata: Age Group, Sex, Ethnicity, Race, Rurality, County, and Health Plan. The tool will enable the user to view enrollment across any combination of filters to help extract actionable insights.
The dashboard will allow us to track enrollments in expansion coverage and identify populations that may be enrolling at lower rates (Figure 1). The dashboard includes a feedback collection feature, and updates and improvements will be incorporated over time. The first iteration of the dashboard launched to the public on December 20, 2023, to track enrollment by demographic group. A future iteration of the dashboard (with a planned release date of 6 to 12 months after expansion launch) will showcase service utilization metrics to provide a better understanding of services being delivered to expansion beneficiaries. The specific utilization metrics are still being finalized but are being modeled after the Louisiana Medicaid Expansion Dashboard.1
NCDHHS has also identified indicators of health access equity, another one of the guiding principles established in our expansion approach. One health access measure we identified is enrollment tracking, the purpose of which is to identify areas of the state that are lagging in the number of beneficiaries enrolled so that extra support and resources may be deployed. NCDHHS is committed to ensuring that all individuals who have become eligible for Medicaid can successfully enroll. To track this, the Data and Evaluation Workgroup is working with the Cecil G. Sheps Center for Health Services Research at UNC-Chapel Hill to develop estimates for the expected distribution of enrollment following ramp-up of Medicaid expansion enrollment. We are also considering how to verify if enrollment lag is created by a lack of effective outreach, the rate of beneficiary enrollment, or a combination of both.
As we considered the populations impacted by Medicaid expansion, we spoke with access and equity professionals who identified the population affected by opioid use disorder (OUD) as a group with the potential to experience outsized impact. We determined that tracking the number of OUD diagnoses and claims will allow us to compare the services provided and determine if the new expansion population is receiving OUD services at a rate equitable to the existing Medicaid population.
We are also in the process of creating a databook of Medicaid expansion metrics to facilitate any expansion-related research and to help monitor expansion as time goes on. This databook includes a subset of measures used in Montana’s Medicaid expansion impact reporting, as well as metrics that have been identified as essential to monitoring expansion in North Carolina. These metrics will be pulled from NCDHHS-level strategic goals, longstanding Medicaid metrics, and new metrics to monitor activities within the agency that are essential to the successful implementation of expansion and its continued improvement.
To ensure accountability among the various divisions within NCDHHS and external partner organizations participating in our workgroups, we established goals for launch, 90 days post launch, and 365 days post launch. Goals were written as statements of the desired results of each group and designed to foster clear understanding of what constitutes success. We used the SMART (specific, measurable, achievable, relevant, and time-bound) approach to build consistency for the cross-divisional work within NCDHHS through clearly defined criteria. SMART goals with specific data requirements were evaluated by our Data and Evaluation Workgroup for feasibility. Goals are tracked using a tool to document progress along the way and monitor potential risks. Goals with the highest impact were prioritized and presented to NCDHHS leadership on a weekly basis.
As NCDHHS continues to make progress toward our 90-and 365-day goals, we will use feedback from our community partners and data (e.g., from our expansion dashboard) to refine and shift our goals as needed.
Using Qualitative Data
Over the past few years, efforts related to the COVID-19 pandemic highlighted the importance of engaging trusted community partners in activities and decisions made by NCDHHS. Early in the planning stages of expansion, we convened five workgroups consisting of NCDHHS leadership from multiple divisions within the department and representatives from a wide range of community partner organizations across the state. Four of our workgroups have a focus area that is in alignment with the overarching strategic goals: Member Enrollment, Health Access, Data & Evaluation, and Communications. Our fifth workgroup, External Implementation Partners, has the overarching responsibility to be a conduit to external partners to provide and receive information that will support Medicaid expansion. In an effort to further broaden our engagement strategy with community partners who are not part of our workgroups, we developed a Community Network Map of organizations based on the type of organization and population(s) and location(s) served. In addition to helping share information with the community about Medicaid expansion, we plan to utilize this community network to reach underserved populations identified in our enrollment-tracking exercise.
The COVID-19 pandemic also put a notable strain on our local Department of Social Services (DSS) offices, as it negatively impacted their workforce. Additionally, our DSS offices across the state are dealing with an increased workload due to the unwinding of the Medicaid continuous coverage requirement and an increased interest in applying for Medicaid due to expansion. To provide support for DSS and to assist with outreach efforts, NCDHHS also developed the Medicaid Ambassador initiative, a statewide strategic network of trusted community organizations whose role is to provide individuals with local support to navigate Medicaid and the online application process. Medicaid Ambassadors are volunteers who support North Carolinians by providing access to technology, providing navigational guidance in our Electronic Pre-Assessment Screening Service (ePASS) portal, answering questions about the application process, and referrals to other resources as needed. Medicaid Ambassadors are meant to serve as a resource for individuals interested in applying who want an alternative to calling or visiting their local DSS.
In addition to the UNC Sheps Center for Health Services Research, NCDHHS has partnered with several other academic organizations to further our expansion-related work, including the Duke University Margolis Center for Health Policy, on an environmental scan of other states that have implemented Medicaid expansion to garner inspiration and direction for evaluation and other activities. States studied must meet the following criteria: similarities to North Carolina in population and political context, a mix of early and late expansion adopters, opportunities for state collaborations, and availability of expansion-related information online. We are in the process of defining data sources, measurement timelines, and owners of the various analyses to ensure evaluation questions results in meaningful findings.
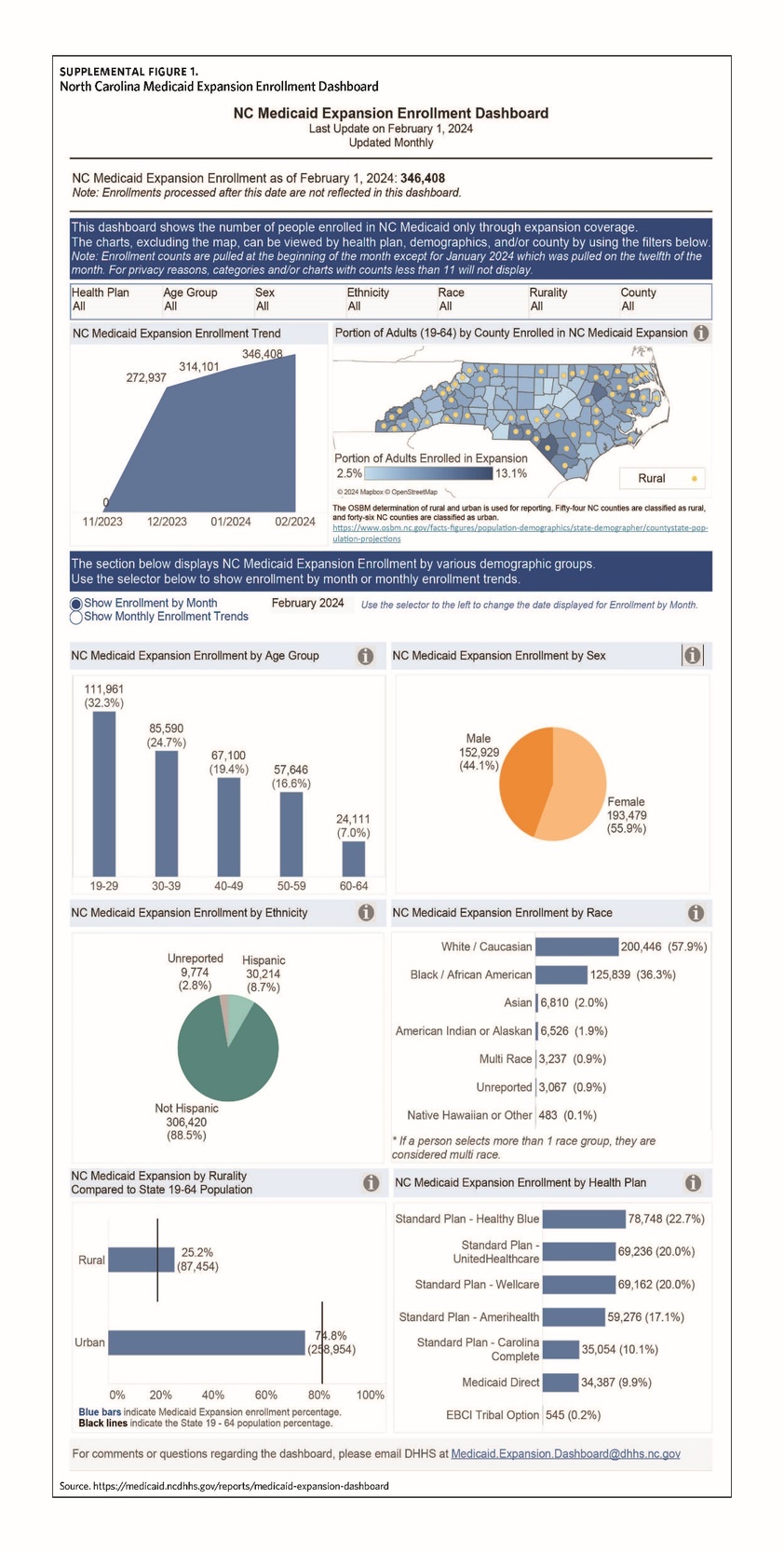
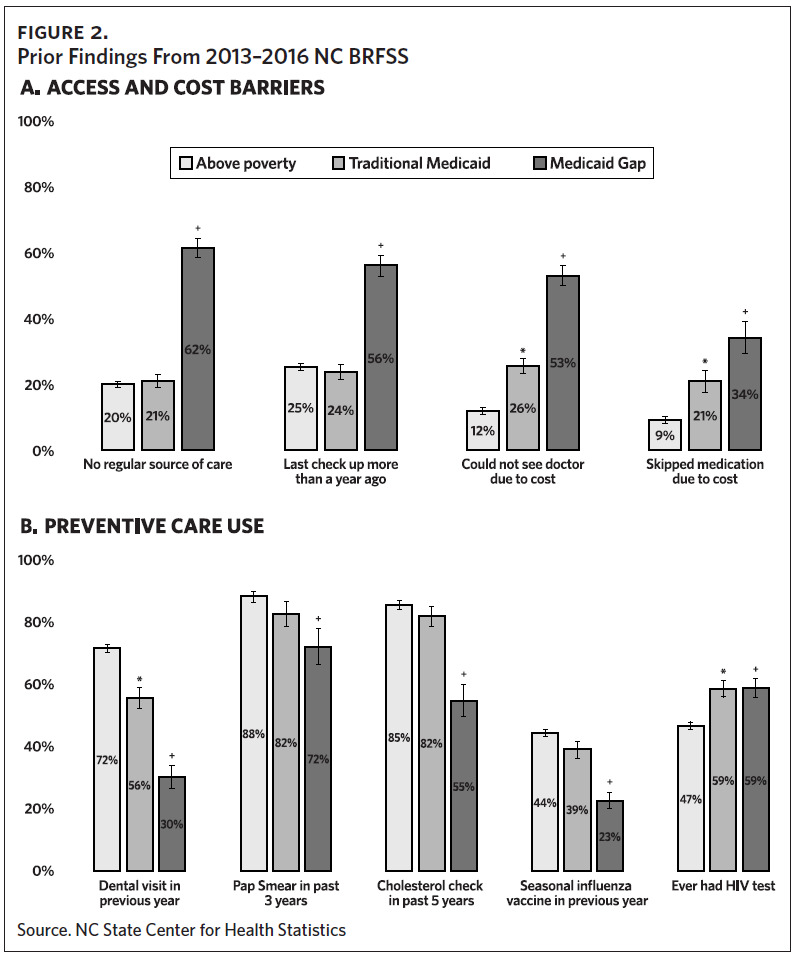
We are also partnering with Duke Margolis, the University of Texas at Austin (UT-Austin), and the State Center for Health Statistics in North Carolina’s Division of Public Health to add and augment questions in future implementations of the Behavioral Risk Factor Surveillance Survey (BRFSS). Analyses will compare prior years’ responses for the population anticipated to become eligible for expansion to that population’s responses after expansion is in place on questions related to access to care and use of health care services—especially preventive services. Our partners at UT-Austin provided 2013–2016 survey data from the BRFSS.
A presentation given to the Data and Evaluation Workgroup on September 18, 2023, by Jenny C. Spencer, demonstrated, “large discrepancies in care access by multiple measures–including being much less likely to have a regular source of care or a recent checkup and being more likely to report cost barriers. There were also gaps in use of preventive care for the Medicaid gap population– including dental care, Pap smear, cholesterol check, and seasonal flu vaccines”2 (Figure 2).
NCDHHS plans to use the aforementioned survey analyses to evaluate the impact of expansion on filling these care gaps.
Conclusion
Using a rigorous and thoughtful approach, NCDHHS developed early guiding principles and a governance structure to begin the work of launching Medicaid expansion in North Carolina. Leaning on critical lessons learned during the COVID-19 pandemic, the department created a governance structure that embedded external partners to guide the work. A thoughtfully executed and data-focused evaluation plan was in place prior to the first member being enrolled, and a public-facing dashboard will allow transparency and access for anyone interested in monitoring the success of North Carolina in achieving our objective to minimize health care coverage gaps and increase access to care for North Carolinians. Teams across NCDHHS and research partners across the country will be monitoring the successful execution of one of the fastest expansions of any state, building on the important lessons our predecessors made available to us.
By measuring the impact and sharing our success with our critical partners, North Carolina hopes other Southeastern states will follow in making more health care available to more people through similar expansion efforts.
Acknowledgments
No conflicts of interest were disclosed.