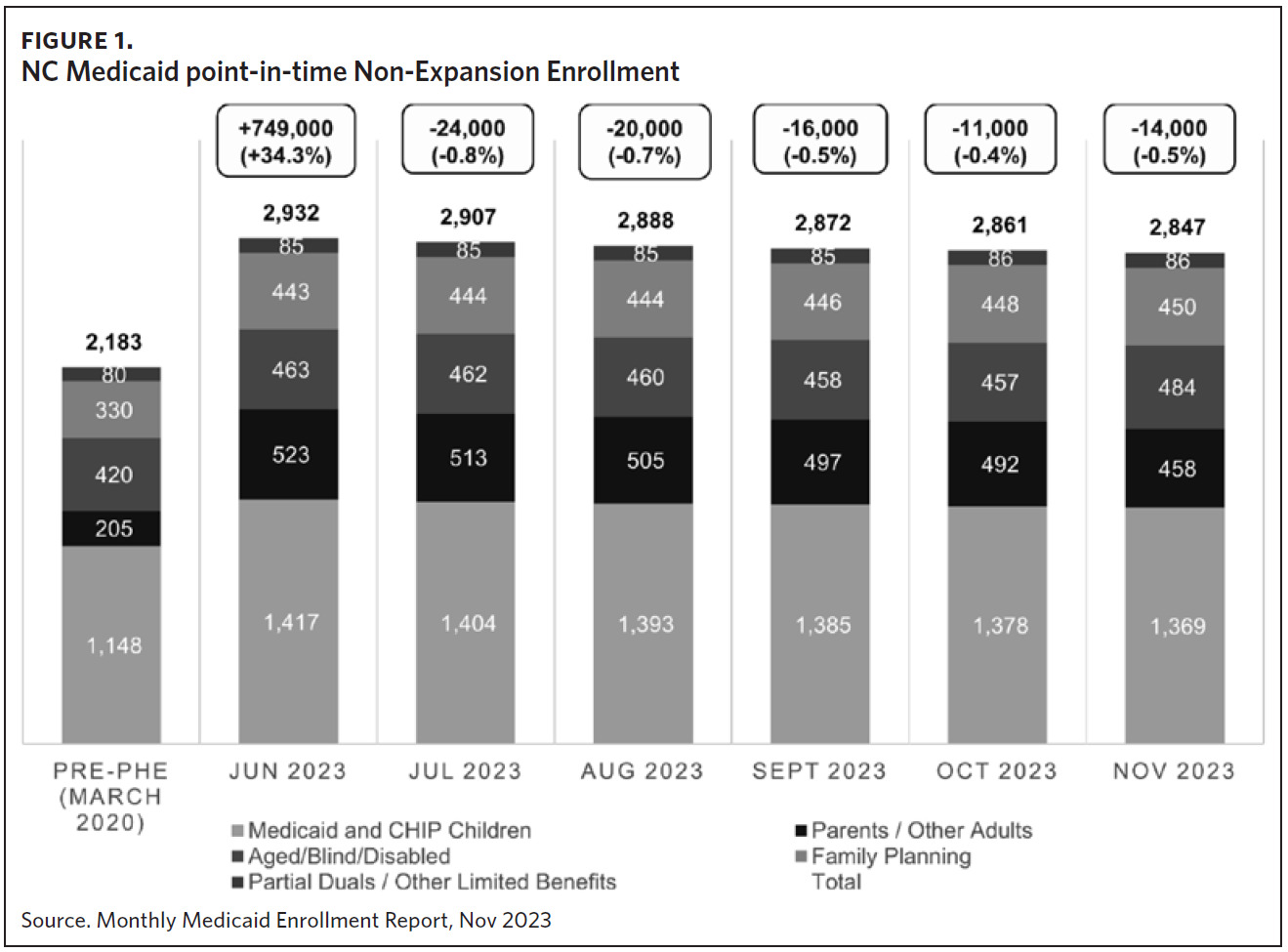
As of February 2024, NC Medicaid provides health care coverage for more than 2.9 million North Carolinians. The COVID-19 pandemic, a once-in-a-lifetime public health emergency (PHE), created historic unemployment in North Carolina as businesses shuttered, staff were laid off, or people left the workforce out of concerns for their health and safety. When unemployment is high, Medicaid enrollment increases as more people have incomes that fall below eligibility limits. Throughout the pandemic, NC Medicaid enrollment grew by almost 750,000 people, largely parents and their children. At the same time, the federal Families First Coronavirus Response Act (FFCRA) of 2020 included a requirement that state Medicaid programs keep people continuously enrolled through the end of the COVID-19 PHE to provide access to health care and COVID-19 vaccines, testing, and treatment. People who may have otherwise lost coverage due to changes in income, family situation, or age kept coverage continuously, increasing our overall caseload from about 2.18 million beneficiaries in March 2020 to more than 2.9 million beneficiaries in June 2023 (Figure 1).
Medicaid Enrollment
North Carolina has a federally regulated, state-supervised, county-administered social services system. Medicaid eligibility and recertifications are determined by 100 county Departments of Social Services (DSSs) across North Carolina and two Tribal offices. The federal government authorizes national programs and funding, the state provides eligibility oversight and support, and local social services agencies deliver services and benefits. County DSS offices are required to accept applications and recertifications in person and via telephone, mail, fax, and online through our Electronic Pre-Assessment Screening Service (ePASS) portal or HealthCare.gov. County DSSs are the public face of NC Medicaid in communities, the front door to benefits and support, and trusted sources of information.
During the pandemic, county DSS offices experienced historic staffing shortages like other industries serving the public and those requiring in-person attendance. Retirements and resignations resulted in the loss of experienced caseworkers, expertise in eligibility policy and systems, and productivity. Due to the lack of qualified applicants, training, and salaries needed to recruit people to these critical frontline jobs, hiring staff was difficult. Bordering counties competed for a limited workforce, and different hiring scales and work requirements left some counties seriously understaffed.
Counties are federally required to process most applications within 45 days, and state law holds counties financially accountable for any health expenditures paid for individuals who were inaccurately determined eligible, meaning that if the county inappropriately approves a person for Medicaid, the county is required to pay back the Medicaid health care costs for that individual. Therefore, training, speed, and accuracy are required in these roles, and many counties struggle in the best of times to find necessary qualified staff.
Medicaid “Unwinding”
On December 29, 2022, Congress passed the 2023 Consolidated Appropriations Act (Omnibus Bill),1 removing the continuous coverage requirement beginning in April 2023. State Medicaid programs were no longer required to maintain continuous coverage for beneficiaries and were required to redetermine all existing beneficiaries, terminating those who were no longer eligible.
On April 1, 2023, North Carolina began what state Medicaid programs refer to as continuous coverage unwinding (CCU), terminating or reducing benefits for people no longer eligible for full coverage per federal law. North Carolina began recertifications for individuals up for renewal by June 30, 2023, so the first individuals in more than three years to lose coverage or receive reduced benefits did so starting July 1, 2023. Immediately, the North Carolina Department of Health and Human Services (NCDHHS) focused on accelerating automation improvements, policy changes, financial support, and training and engagement opportunities to help counties meet this increased demand.
Medicaid Expansion
After over 10 years of advocacy, Medicaid expansion passed the North Carolina General Assembly and was signed into law by Governor Roy Cooper on March 27, 2023. Session Law 2023-7 (House Bill 76) tied the effective date of Medicaid expansion to the enactment of the state budget,2 so an implementation date was still pending as counties began to feel the gathering of “the perfect storm.” Caseloads were higher than ever in the history of the NC Medicaid program, and county DSS offices were experiencing the highest staffing shortages. Over 600,000 individuals are estimated to be enrolled in Medicaid expansion over the next several years.
NC Medicaid implemented several technological improvements to reduce the county DSS workload. The first and most impactful automation was NC Medicaid’s systematic assessment of individuals currently enrolled in Medicaid’s limited benefit Family Planning Program (FPP) for eligibility in the new Medicaid expansion full benefit program. Through automation in NCFAST, the North Carolina eligibility and enrollment technology platform, more than 260,000 beneficiaries were automatically enrolled in Medicaid expansion on December 1, 2023, with no county action required (unpublished data, NC Medicaid).
Streamlining Recertifications and Applications
NC Medicaid also focused on automating recertifications and applications with straight-through processing (STP) that requires no county action. Prior to this change, while the eligibility system automated many steps of the process, county caseworkers reviewed every piece of evidence on a case and were required to approve the determination before it could be fully processed. Today, all applications and recertifications approved by the system in which beneficiaries keep or increase their coverage are processed without caseworker review. Any reduction in benefits or terminations still require caseworker review to ensure beneficiaries are not incorrectly losing coverage. Long a priority, the CCU and looming expansion helped expedite systems changes to increase STP percentages, resulting in a current monthly average of 56,000 applications and recertifications requiring no touch (unpublished data, NC Medicaid).
As part of the CCU, federal law requires states to use multiple modalities of communication to encourage beneficiaries to provide updated contact information during the recertification process. NC Medicaid implemented an automated proactive communications solution to communicate key messages, requests for information, and reminders through text messages, email, and automatic phone calls. Additional automation efforts included receiving approval from our federal partners to use updated Food and Nutrition Services (FNS) information for individuals receiving that benefit to automatically determine Medicaid eligibility. Finally, NC Medicaid became a federally facilitated marketplace determination state on February 1, 2024.
Policy Changes
There are several policy flexibilities the Centers for Medicare & Medicaid Services (CMS) allows states to use to increase recertification processing. North Carolina implemented every policy flexibility available and applicable to streamline workloads, including:
-
Updating beneficiary addresses using the U.S. Postal Service forwarding address or National Change of Address (NCOA) without additional verification. Previously, caseworkers were required to contact beneficiaries individually via mail and telephone to confirm address changes;
-
Increasing the “reasonable compatibility” threshold for data matches from 10% to 20% to help increase application processing. Prior to the change, information returned from data sources that fell outside of the “reasonable compatibility” range resulted in additional requests to beneficiaries for information via mail that were initiated by caseworkers, slowing down processing times; and
-
Automatically renewing Medicaid eligibility for individuals over age 65, adults with disabilities, and adults who are blind who have incomes at or below 100% FPL and asset amounts below the reserve limit, beginning in January. Prior to this policy change, beneficiaries would be required to verify any changes in income or assets and respond to a notice sent by a caseworker requesting additional information. This flexibility allows eligible beneficiaries to retain coverage without providing additional information.
Finally, and perhaps most impactful, NC Medicaid received a waiver from CMS to extend eligibility for 12 additional months for all children under age 19 starting in December 2023. Continuing health care coverage for children is in the best interest of their health outcomes.3 Rather than losing coverage, children—who comprise half of the 2.8 million North Carolinians enrolled in NC Medicaid—will have access to full Medicaid benefits for another year without any action required. Extending their recertification date by 12 months has the added benefit of significantly reducing the workload of county DSS staff so they can focus on adult recertifications and new applications for coverage.
Financial Support
In June 2023, in response to requests from county leaders, NCDHHS distributed $8.335 million in funding to counties to support efforts to prepare for expansion implementation before the funding from the Medicaid expansion legislation became available. This funding allowed counties to hire and train staff, purchase computer and office equipment, lease space, and even provide overtime and incentives for existing staff.
In accordance with Session Law 2023-7, NCDHHS began distributing an additional $1.667 million per month to counties to support Medicaid expansion on December 1, 2023. Per legislation, the funding to counties is set to increase in subsequent years and will be indexed to inflation. The funding covers the county share of eligible Medicaid expenditures. Additional federal dollars are drawn to match the county share, so the total amount of funding is 50% to 75% percent more, depending on the type of expenditure.
Training and Engagement
NC Medicaid has prioritized and increased training opportunities and technical assistance to help bolster the county DSS workforce by:
-
Providing targeted technical assistance to the counties on process improvements and workflow enhancements through multiple on-site meetings;
-
Conducting quarterly county surveys to collect data on staffing, vacancies, application/recertification progress, and call volume;
-
Conducting Medicaid expansion and recertification process training;
-
Convening a monthly DSS County Workgroup on expansion and the CCU since 2022;
-
Increasing the frequency of on-site county visits made by NC Medicaid Operational Support Team (OST), who work with all 100 counties to provide policy clarifications, process improvements, training, and assistance with corrective action plans;
-
Providing 30 statewide best practice recommendations;
-
Distributing a County Staffing Tool to counties to estimate the number of staff required for applications and recertification processing depending on caseload; and
-
Creating an internal monitoring report (IMR) to track application and recertification progress by county so that counties can see their staff work throughput and processing backlog.
To increase the number of applications processed automatically and reduce county workload, NC Medicaid conducted and recorded step-by-step application demonstrations in English and in Spanish for community organizations using the Electronic Pre-Assessment Screening Service (ePASS) portal.4 An accompanying reference guide provides additional information. In addition to application assistance materials, NC Medicaid developed a Medicaid expansion toolkit for distribution to health plan partners, community organizations, county DSSs, interested stakeholders, and the public to help promote awareness of the increase in coverage.5 The online toolkit includes downloadable flyers on Medicaid expansion, Medicaid services, and Medicaid expansion’s interaction with the federal HealthCare.gov plans, as well as approved presentations for community events, reusable social media images and messages, and newsletter templates for community and faith organizations to use. NC Medicaid also has a portal for stakeholders to sign up for updated information on Medicaid expansion so approved messages are disseminated widely.5
NCDHHS also organized a statewide External Implementation Partners Workgroup to focus on Medicaid expansion implementation. A coalition of advocates, providers, community organizations, governmental organizations, and philanthropic donors met together and in subgroups to support counties, health care providers, and community organizations interested in helping with Medicaid expansion implementation. The Member Enrollment Workgroup, the Health Care Access Workgroup, the Data and Evaluation Workgroup, and the Communications Workgroup met biweekly in the months preceding Medicaid expansion launch to develop key messages for trusted community voices to use to reach individuals who may not be aware of the benefits of Medicaid expansion. More than 350 organizations are trained to give presentations on Medicaid expansion in English, with another 100 organizations trained to give presentations in Spanish. Volunteers—including state and county public libraries, community colleges, faith groups, legal aid organizations, coalitions serving the Latinx population, and many others—attested to having watched the ePASS demonstration and listed themselves as Medicaid Ambassadors for individuals seeking assistance applying for Medicaid. The Medicaid Ambassadors contacts were shared with county DSSs as community resources and will be listed on the Medicaid.nc.gov website in early 2024.
CCU and Medicaid expansion provided NC Medicaid with an historic opportunity to prioritize systems changes and streamline county DSS workloads, policy changes to increase workflows, funding to hire and retain staffing, and training and engagement so that North Carolinians have the resources they need to apply for Medicaid. Enrolling North Carolinians in Medicaid expansion is a long-term project, and NC Medicaid remains committed to making sure county DSSs have the support they need to get and keep North Carolinians covered.
Acknowledgments
No conflicts of interest were disclosed.