Social drivers of health (SDOH) are social and economic conditions that influence the distribution of resources and shape downstream individual health and social needs.1 These social conditions—including social isolation, unemployment, food insecurity, and housing instability—affect health outcomes, quality of life, and equity. The COVID-19 pandemic has accelerated calls for action due to the resulting expansion of existing inequities in social and health outcomes.2,3
Investing in social care interventions that respond to unmet needs using local resources and social assistance programs can be less costly and more effective than repeated intensive medical interventions.4–8 Food insecurity, for example, reduces dietary quality, increases stress, and impedes health self-management due to cost barriers to healthy eating. Recent research suggests that participation in the Supplemental Nutrition Assistance Program (SNAP) as a food insecurity intervention is associated with lower subsequent health care expenditures.4
As health care systems transition toward value-based payment arrangements, they are incentivized to adopt care models that are responsive to both medical and social needs.9–11 Growing from their infancy over the past decade, these payment models now account for nearly 41% of all US health care payments.12 As a result, payers have launched initiatives to address patients’ unmet social needs through social and medical care coordination to control health care costs while improving quality.10,13,14
Accelerating efforts to improve social and medical care coordination requires initiatives that screen for and address social needs.15,16 Despite notable progress in screening for social needs, challenges in care coordination between health and human service organizations persist. For example, staffing constraints inhibit the ability to provide case management that helps navigate administratively complex social service programming and community resources.17 Similarly, identifying an adequate referral network of agencies or resources that can address identified needs is time and resource intensive.18 A shared technology platform is a potential solution that can help overcome fragmented health and social service provision and may help facilitate referrals and case management.19
To promote adoption of social needs screening and response across health care and community settings, the North Carolina Department of Health and Human Services (NCDHHS) introduced NCCARE360, the nation’s first statewide digital health and social care coordination platform.20 Implemented on the UniteUs technology infrastructure, NCCARE360 creates a shared, secure network to send and receive electronic referrals and track client outcomes across North Carolina. While most patients are referred by health care workers or community-based organization (CBO) staff, individuals can also contact NC211, an existing free and confidential information and referral service offered through United Way of North Carolina. Through NC211, individuals can request a referral and case management through the platform via telephone or internet.
NCCARE360 has three primary functions: 1) to provide an updated community resource directory made up of services offered by locally available social service agencies, CBOs, and health care organizations; the platform can be used by existing United Way NC211 infrastructure consisting of navigators, call centers, and data teams to correctly maintain community resource information21; 2) to operate as a secure, shared platform for health care and human services providers to match and refer eligible, consenting individuals to resources and assistance and respond to their unmet needs; and 3) to “close the loop” on referrals by providing real-time data, feedback, and referral status outcomes and service initiation across organizations.22 For example, if an individual reports food insecurity, a member of their health care team can refer the individual to resources and services they are eligible for on the platform (e.g., the local food pantry) and assess whether and when assistance was received. This closed-loop communication is facilitated by the flexible architecture that permits integration for referrals through the platform while preserving common privacy and security standards (i.e., HIPAA, FERPA, and FIPS).1
NCCARE360 began rollout in select North Carolina counties in 2019 and became available in every county in June 2020. As of January 2023, NCCARE360 had onboarded over 3,055 organizations and served approximately 115,000 clients.23 NCCARE360 was introduced to complement existing programs and reforms to the state Medicaid program. For example, the NCDHHS plan for managed care transition was to include NCCARE360 as part of the 1115 Medicaid waiver. The state Medicaid program’s transition to managed care features universal social needs screening of Medicaid beneficiaries to identify food and housing insecurity, transportation access, and interpersonal violence.24 NCCARE360 is being deployed to support service delivery of the waiver program’s major initiative, the Healthy Opportunities Pilots, a $650 million investment to finance and evaluate the impact of social care interventions on health and cost.20,25 Additionally, NCCARE360 was incorporated into an emergent NCDHHS program to address health-related social needs during the pandemic— the COVID-19 Support Services Program (COVID-SSP).26
NCCARE360, universal social needs screening of Medicaid beneficiaries, the Healthy Opportunities Pilots, and initiatives like COVID-SSP are representative of an emerging policy trend of systematic data collection and social care activities among state Medicaid programs across the country. Of 40 states that provide Medicaid services through risk-based managed care plans, 35 include social needs screening, referral, and care coordination activities.27 Thus, there is a need to identify best practices for doing so within existing care pathways and as part of an overarching population health management strategy.
This report will describe NCCARE360, present initial implementation results within a large integrated health system and surrounding community, and highlight practical, multi-level considerations to inform adoption and scaling. We collated frontline stakeholder experiences and recommendations across the individual, organizational, and policy levels to evaluate the current experience and future potential of NCCARE360 to improve population health and equity. Our findings can inform other states, payers, and organizations adopting similar technologies to better coordinate health and social care activities.
Methods
COVID-SSP Case Study
Preliminary data from Durham County provide a case study of people’s experience using NCCARE360. Durham County, with a population of 326,126 people, is majority populations of color (36.9% African American, 13.7% Hispanic or Latino, 43% White)28; 14% of the population lacks health insurance and 11.7% of people within the county live on incomes below the federal poverty limit.29 In Durham County, 7,649 clients have had referrals placed across 153 unique organizations using NCCARE360,23 though Durham County is not a region of the state selected to receive social care reimbursement through the Healthy Opportunities Pilots. The NCCARE360 launch included adoption by the largest integrated health system in the county, Duke University Health System (DUHS). DUHS adopted social needs screening and response using a variety of approaches, including where screening occurred, the modality used, team members responsible for consenting patients and placing referrals, and situations in which additional case management was offered.
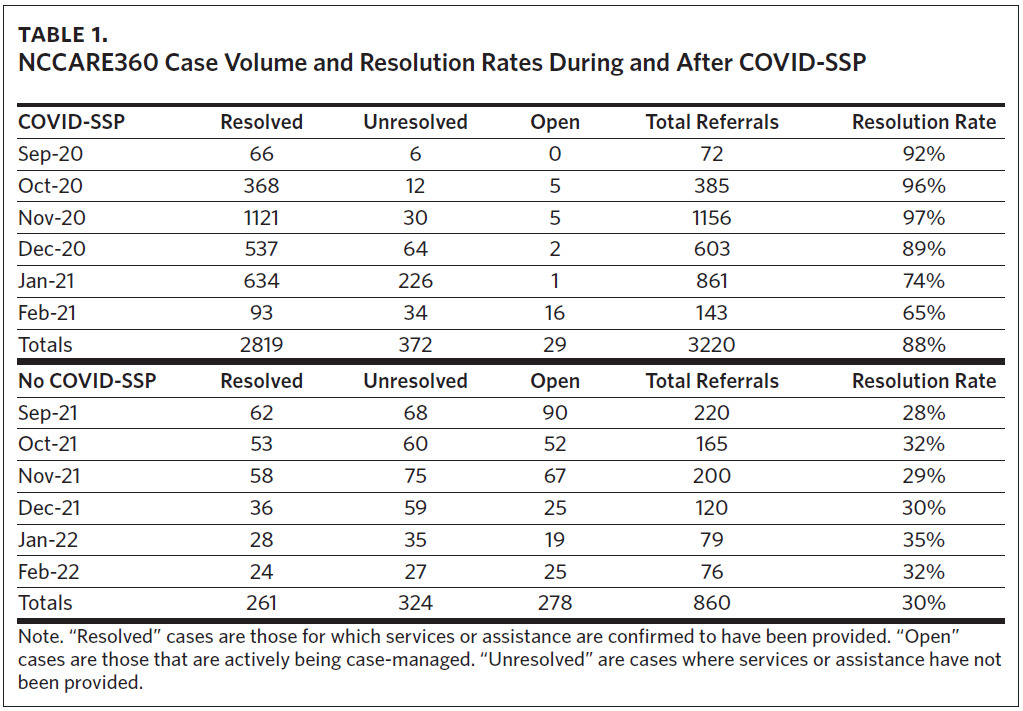
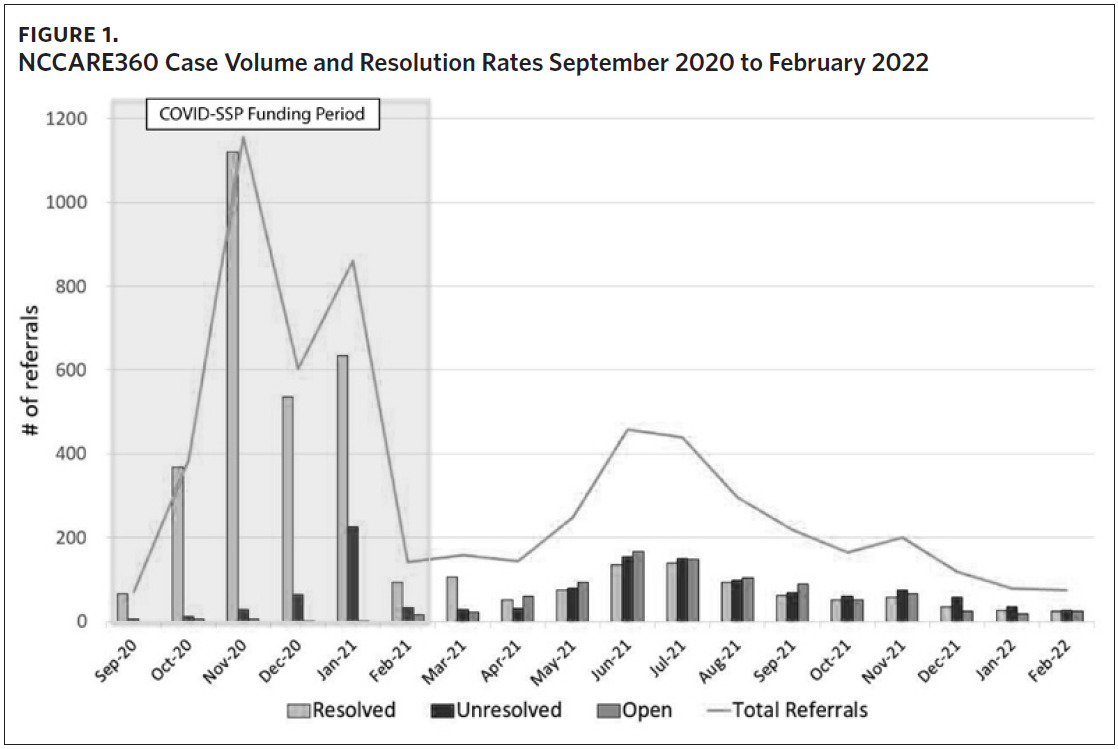
To understand the platform’s feasibility and performance, we considered case-resolution rates using NCCARE360 in Durham County with and without COVID-SSP funding. The first time frame was during the fall of 2020 (September 1, 2020 to February 28, 2021) when COVID-SSP was implemented. COVID-SSP provided funding across 34 counties to supply services to vulnerable, low-income individuals, enabling recipients to successfully quarantine, isolate, or shelter in place during the pandemic. COVID-SSP leveraged funding from the Coronavirus Aid, Relief, and Economic Security (CARES) Act and state funding.26 COVID-SSP involved a food needs assessment, with food box delivery and in some cases financial relief for those in need. Eligible individuals included those who tested positive for COVID-19, were exposed to COVID-19, and those who were at high risk for COVID-19 death or hospitalization who would not be able to quarantine without assistance. Importantly, COVID-SSP provided reimbursement to specially designated CBOs for the provision of services, telephonic outreach, and case-management activities (e.g., assessments and referrals) by community health workers (CHWs) through NCCARE360. CHWs and clients reported positive experiences with COVID-SSP.26 We used referral data from DUHS and the Duke COVID-SSP organizations that provided food assistance and case-management services within NCCARE360 to assess cases and referral resolution rates.
The second time frame was the same five-month period the following year after the COVID-SSP funds were exhausted and reimbursement for assistance and case management activities ended through NCCARE360. We compared referral resolution rates between these time frames to highlight the important role of having dedicated reimbursement mechanisms in the platform’s use and referral resolution rates. Data were abstracted from the UniteUs Insights Center on September 2, 2022. This evaluation was submitted to and deemed exempt by the Duke University Health System Institutional Review Board (Pro00110154).
Results
We found that when COVID-SSP funding was available, the referral resolution rate (i.e., reported as resolved by the organization that the individual was referred to) was significantly higher (88% resolved) for COVID-SSP-approved CBOs than during the same five-month time frame after COVID-SSP funds were exhausted (31% resolved) (Table 1). The lower volume of referrals and resolution rates after COVID-SSP funds were exhausted is part of a clear trend when examining NCCARE360 data from the entire time frame from September 2020 through February 2022 (Figure 1). When coupled with existing evidence of high levels of satisfaction among clients and CHWs,26 these findings highlight critical policy considerations surrounding the financing of social care integration. Specifically, policy mechanisms to reimburse for provision of food assistance have dramatically affected CBOs’ ability to resolve, or “close,” cases in real time. Notably, while dedicated reimbursement mechanisms can improve the ability of CBOs to respond to unmet social needs, the lagging retrospective reimbursement required CBOs to use existing personnel and capacity to scale. Based on CBO stakeholder feedback, this may have hindered the ability for these small organizations to mobilize more rapidly to meet demand for these services.26
Discussion
NCCARE360 uptake and referral resolution rates varied dramatically depending on the presence of a dedicated reimbursement mechanism for CBOs and social service providers. These results are subject to several limitations.
First, we caution against generalizing our findings to other counties and regions of the country. Second, the uniqueness of this period during the pandemic and co-occurring challenges related to health and economic conditions leaves these results vulnerable to bias. Referral volume and resolution rates may have been impacted by unmeasured or confounding variables other than COVID-SSP funding.
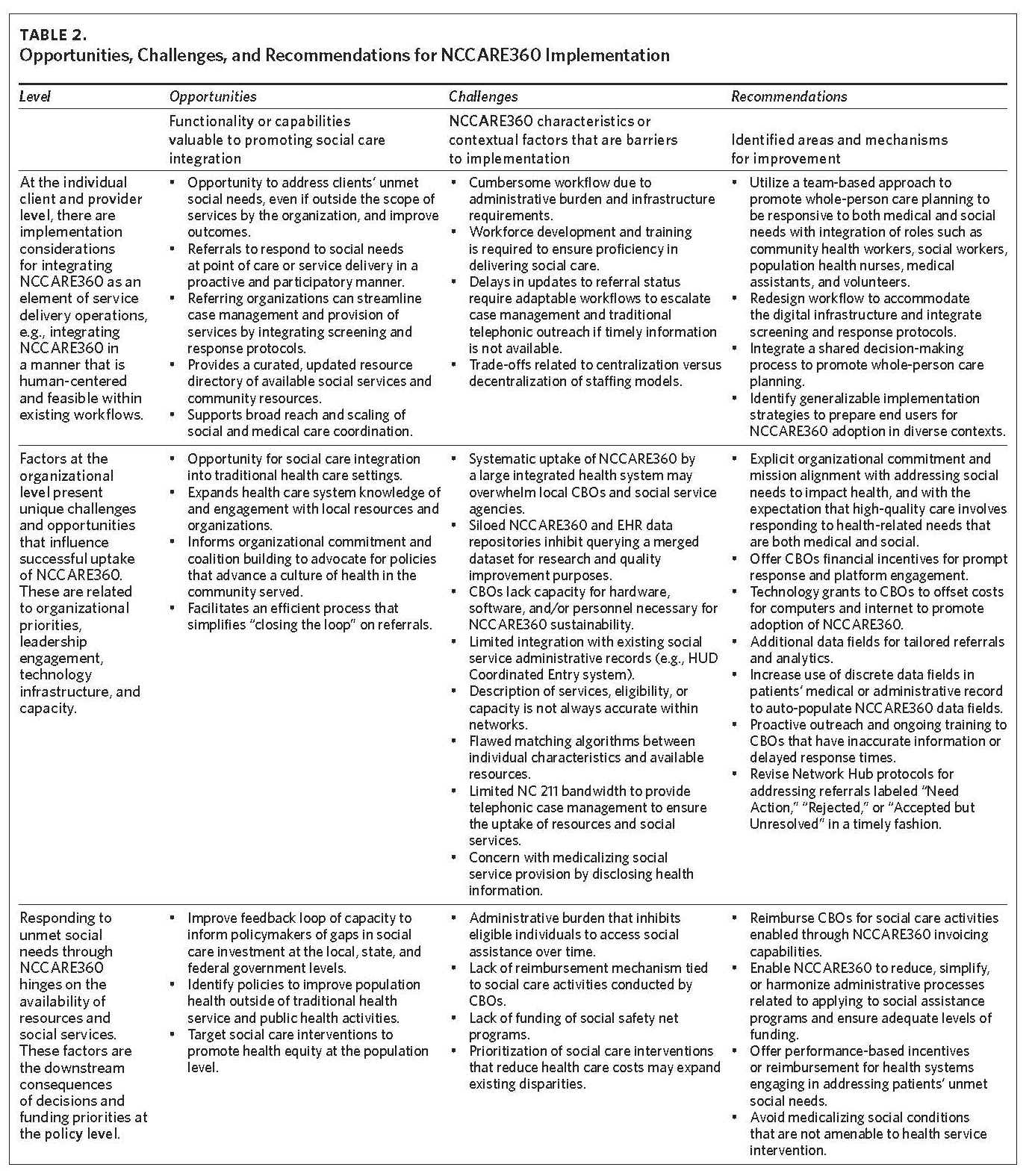
To interpret and contextualize these findings, we describe the implementation experience and recommendations of public health professionals, CBO leaders, clinicians, researchers, and frontline users of the platform across multiple levels (i.e., client-provider, organization, and policy). These findings have been further detailed in Table 2 to describe NCCARE360 opportunities, challenges, and recommendations across the client and provider, organization, and policy levels. These multilevel perspectives were derived from health system and county-level community advisory group meeting minutes. Advisory groups consisted of representatives from CBOs, the county public health department, and clinical stakeholders from throughout Durham County. Agenda and meeting minutes (available upon request) were abstracted into a matrix to identify themes and patterns.
Client- and Provider-Level Considerations
Integration of health and social services starts with a commitment to addressing patient needs through partnership and communication with service organizations. For example, the Centers for Medicare and Medicaid Services (CMS) highlights the importance of health care providers being responsive to patients’ values and preferences to support self-management beyond traditional boundaries of clinical care.30 Novel team-based models of health care delivery ensure a wider breadth of services to address both medical and health-related social needs. Although NCCARE360 represents an opportunity to use technology to streamline these services, addressing social risk requires workflow redesign to screen and respond to social needs in an equitable, human-centered manner.
Embed adaptable social needs screening and response protocols into workflows. Integrating NCCARE360 involves the adoption of systematic screening for social risk at a service encounter to enable the identification of unmet needs, documentation, and subsequent referral. Flexible workflows for screening include a variety of modalities (e.g., paper, tablet, direct interview) that enhance adoption and involve electronic health record (EHR) documentation to improve whole-person care planning with social and economic considerations.15,31,32 However, the cost of implementing and maintaining response workflows may be a barrier to implementation.33 Based on our experience with NCCARE360, we recommend a continued focus on scaling specific social care interventions or community resources (e.g., improving enrollment in social safety net programs or assistance programs specific to a local context) that are available, effective, and stand to realize the greatest improvements in health equity.
Compared to previous conventional case-management outreach, NCCARE360 represents unique benefits and efficiencies that support operating at scale across an entire state. This includes improvements in “closing the loop,” a process that previously relied on labor-intensive telephonic case management with little ability to consistently confirm referral outcomes. However, despite the promise of NCCARE360 to support this function, many participating organizations have continued telephonic case management due to lack of timely referral follow-up within NCCARE360.
This may be due to inadequate staffing to update the status of the case within the platform or due to user error.
Embrace novel models of team-based care. NCCARE360 and corresponding workflows benefit from a team-based approach with defined roles and meaningful input from the patient or client.34,35 The breadth of roles required to address social needs has substantial implications for workforce development and care team composition.36–40 Experiences with NCCARE360 suggest that personnel background can vary, but effective response requires technology-specific training (e.g., workflow planning meetings, software training sessions) and knowledge about local social service delivery (e.g., roles of social services, program eligibility, community resources). Further, mistrust of medical and social service institutions, particularly among undocumented and historically marginalized communities, is a challenge to the equitable implementation of NCCARE360. Unique skill sets and competencies are required for assessing social needs and making appropriate referrals, including stigma reduction, confidentiality maintenance, empathic communication, motivational interviewing, and language access. Also, knowledge of the community, accessibility, and willingness to invest in establishing trust with members of the community are important skill sets.17,38,41 For example, NCCARE360’s success with the COVID-SSP during the COVID-SSP’s first phase was partially dependent on the substantial CHW workforce developed and deployed by the NCDHHS CHW Program. However, training CHWs for NCCARE360 was hindered by English-only materials that furthermore were not written at an appropriately lay-friendly reading level.26 NCCARE360 and similar technologies broaden the definition of a care team outside of the traditional boundaries of health care systems, public agencies, and CBOs, but more attention to accessibility and technology-specific training is required to fully realize their potential.
Organization-Level Considerations
Organizations including health care systems, quasi-governmental organizations, and nonprofits also contribute to the platform’s success. This includes a broader organizational commitment to embracing community collaboration and advocacy for policies that advance a culture of health.42 Additionally, NCCARE360 is optimized with dedicated resources and personnel who use the technology routinely.
Invest in complementary technology and data-management infrastructure. While NCCARE360 connects patients to community resources, organizations should consider the technology infrastructure necessary to use it routinely. Since NCCARE360 is an electronic platform, small CBOs that have traditionally used paper filing systems have not been able to adopt NCCARE360 due to lack of funding for hardware, software, or personnel. CBOs and social service agencies have highlighted challenges with NCCARE360’s limited integration with existing technologies and systems. For example, NCCARE360 lacks necessary integration with the Department of Housing and Urban Development’s Coordinated Entry system, which is used to coordinate services.43 This fragmentation of technology undermines efforts to coordinate health and social care activities. The costs to integrate NCCARE360 for CBOs are significant (e.g., hardware, internet connectivity, workforce development). We recommend dedicated, sustainable funding mechanisms beyond grants to supplement existing technical assistance and to offset CBO costs for NCCARE360 adoption and continued use.
For health systems, NCCARE360’s web-based version has a limited level of integration with existing EHR technologies, which may present a barrier to systematic use. In contrast to the web-based version, the EHR-enabled NCCARE360 has the benefit of being able to abstract and automatically populate select demographic fields, which supports efficient use in busy clinical settings. We believe there is a development opportunity to identify additional discrete data fields in patients’ medical records, when appropriate, that can be used to auto-populate NCCARE360 data fields. This capability could inform matching algorithms to ensure resources are better targeted to eligible individuals. The lack of better matching algorithms and financial incentive for CBOs to be fully engaged with maintaining accurate eligibility criteria complicate efforts to design efficient workflows and gain provider buy-in.
Enhanced bidirectional flow of relevant health-related social needs and referral status data from NCCARE360 into the EHR will support quality improvement and health services research.
While there is evidence that social needs data are predictive of health risk,44 the fragmented and siloed nature of EHR and NCCARE360 data repositories complicates the application of quality improvement and research methodologies to identify social care interventions that could most benefit patients. The inability to easily merge and analyze longitudinal data from the EHR and NCCARE360 represents a missed opportunity to better understand referral effectiveness in a local context and disseminate promising strategies for addressing intersecting unmet social and health needs.
Promote network health standards and cross-sector communication. Despite the promise of NCCARE360, limited capacity for CBOs and social service agencies to update, interact, and act on referrals in a timely manner has diminished the platform’s impact. Mislabeled and mismatched resources and descriptions of services provided undercut the client experience. To improve the NCCARE360 network, we recommend:
-
Ensuring CBO information is up to date through auditing and incentives;
-
Proactively offering additional and ongoing training to users responsible for maintaining information on available resources and acting on referrals;
-
Ensuring eligibility criteria are easily accessible. Matching criteria could be automated so that search results are filtered based on key demographic variables, including specific factors that might determine eligibility (e.g., insurance types, age, veteran, or disability status);
-
Revising Network Hub protocols for addressing referrals labeled “Need Action,” “Rejected,” or “Accepted but Unresolved” in a timely fashion;
-
Expanding funding for NC211 to build capacity for service navigation for individuals who have unresolved referrals. Navigator services should also prioritize clients with the highest number of intersecting unmet social needs to realize greater impact on equity and outcomes;
-
Providing funding for hardware, software integration, and personnel for CBOs to increase capacity to use NCCARE360.
System- and Policy-Level Considerations
The availability of and process for accessing resources on NCCARE360 is directly influenced by system- and policy-level determinants. Efforts to improve social and health care coordination must be complemented by policies that improve population health.42 This extends to policies that influence the extent to which CBOs and social assistance programs (e.g., SNAP) using NCCARE360 are accessible and adequately funded. The integration of health and social care data and workflow may medicalize social conditions that are not amenable to health service intervention. An unintended consequence could be prioritizing health care-related system-based solutions as opposed to more effective, equitable, and efficient strategies or policy levers to address social needs (e.g., tax, labor, or social welfare policies). If social care interventions are prioritized based on their potential to reduce health care costs, this could lead to a myopic focus on current high utilizers and have the unintended consequence of expanding existing disparities.45
Invest in an expanded and accessible social safety net. Key stakeholders’ experiences with NCCARE360 point to the importance of policy changes that reduce administrative burden and expand investments in the social safety net. In a recent study of a primary care-based screening, response, and telephonic case management intervention in North Carolina, only 32.7% of patients reported service initiation resources within four weeks of the original referral.46 This is consistent with a 2017 systematic review of screening and response interventions, which found that the uptake of resources ranged from 32% to 64%.47 Notably, the most predictive variable of referral resolution was related to the complexity of the applications and enrollment processes to obtain services.46 Ideally, NCCARE360 could alleviate administrative burden, which is a barrier for eligible individuals to access their legally entitled benefits for social safety net programs (e.g., TANF, SNAP, and Medicaid).17,48 This challenge is felt most acutely for housing assistance in North Carolina; however, this challenge is not unique to the state. For example, even for individuals eligible to receive Section 8 Housing Choice Vouchers, less than 30% receive them, and after two years of waiting on average.49
Reimburse for social care activities. Community partners, public agencies, and CBOs have expressed frustration with the increased demand for launching NCCARE360 within health care settings without corresponding investments in local capacity to address identified unmet needs. This phenomenon, sometimes referred to as the “bridge to nowhere,” refers to significant investments made in screening and connecting patients to community-based resources without concurrent and similar investments in CBO or social service capacity; this bridge to nowhere undermines efforts to realize improvement in health outcomes or cost containment.50 Emerging value-based payment models, particularly among state Medicaid programs, seek to incentivize funding of social care through risk-based payments and shared-savings schemes coupled with specific metrics (e.g., requirements to create linkages with social service programs).50 Progress toward reimbursing social care activities by identifying evidence-based interventions is a critical step. The Healthy Opportunities Pilots program initiative launched by NCDHHS in 2022 is the first comprehensive evaluation of evidence-based, nonmedical interventions in the United State.25 It represents an important opportunity to leverage NCCARE360 for making referrals and “closing the loop,” but also provides a mechanism for invoicing clients for provided resources and rendered services. As the evidence base for specific social assistance programs and community resources develops, there will likely be greater momentum toward reimbursing for these services as a defined benefit for enrollees.
Conclusion
While the adoption and rollout of NCCARE360 as a statewide digital social care coordination platform represents an innovative effort to accelerate adoption of social needs screening and response in health care settings, there are several opportunities for improvement. The low rate of uptake of referred services—be it due to administrative burden, lack of funding, or geographic availability—represents a persistent challenge for social needs screening and NCCARE360. To be effective, CBOs and social service providers must have sufficient funding and streamlined processes in order to adequately accept new clients. The COVID-SSP example provides evidence that when CBOs are reimbursed for service provision using the platform, they can scale and respond, amplifying the impact of the NCCARE360 platform. To complement these structural areas for improvement, users of the platform will require training in community context, social resource allocation, and service navigation. Embracing structural solutions to improve access to social services and community-based resources will amplify the benefit of NCCARE360 and support the shift to value-based care, improving health outcomes and equity.
Disclosure of interests
No authors report any relevant conflicts of interest.