Background
Informal caregivers are family members and friends who care for individuals (care recipients) across the life course, from infancy through old age, and across the spectrum of illness and disability. The care they provide is rarely compensated, recognized as critical work in society, or adequately supported or supervised. The tasks caregivers perform vary widely based on the needs of recipients, the resources of their households, the formal clinical support services (such as in-home nursing) available in their areas, and several community and contextual factors of where they reside.1,2 Both national3,4 and North Carolina-specific reports5,6 point toward the harms caregivers can experience when personal and community supports are inadequate to match the emotional, financial, and physical demands of caregiving. These include worsened emotional health,7,8 forgone employment and financial strain,9–11 and adverse physical health outcomes.2,12 In addition, the COVID-19 pandemic has exacerbated many of these adverse consequences of inadequately supported caregiving.13
Caregiving impacts every life domain, including mental and physical health, social relationships, employment, and work. Accordingly, caregiver support systems should be accessible, comprehensive, and integrated. It is in the clear interest of a state and its citizens to ensure that its caregivers are recognized and supported emotionally, financially, and professionally. However, data on caregiver support policies show wide state and regional variation in level of benefits provided, eligibility, and coverage. According to a recent national analysis, North Carolina ranked among the bottom five states in terms of the available caregiver supports based on the National Academies of Science, Engineering, and Medicine’s caregiver support recommendations: unemployment insurance, family responsibility protected classification, paid family medical leave, spousal impoverishment protection, state-level dependent care tax credits, and caregiver training through Medicaid waivers.14
North Carolina has an estimated 1.3 million informal caregivers, accounting for 1.1 billion care hours, an unrealized economic value of $13.1 billion per year.15 The demographics of North Carolina are changing, with increasing proportions in the population of older adults and of children and youth with complex health needs who often need in-home caregiving.14 Currently, North Carolina ranks ninth nationally in total population and eighth in the number of people aged 65 and older.14 Additionally, in the next 20 years, North Carolina’s population aged 65 and older is projected to almost double, from 1.7 to 2.7 million. The growth of the demographic of those aged 85 and older, ages at which higher levels of care are often needed, is projected to be 116%.16 North Carolina also has a higher relative population proportion of children and youth with complex needs (22%) compared with the national average (20%).17
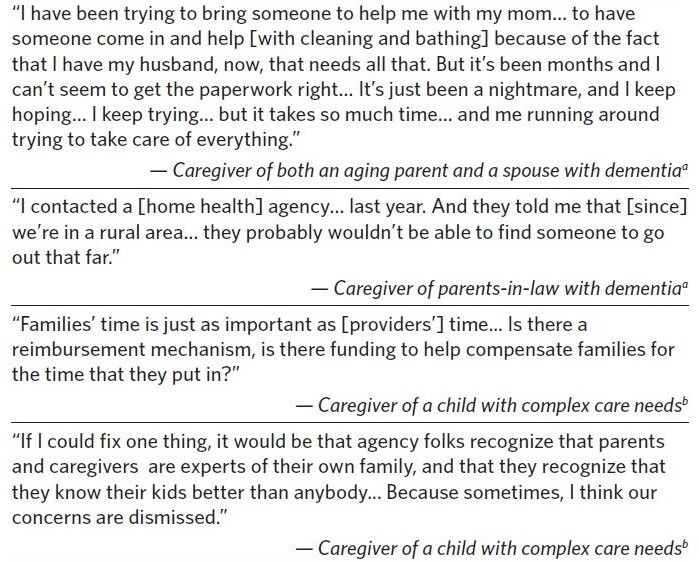
In Caregivers’ Own Words
Statistics tell part of the story, but the words of caregivers make clear the urgency of attention needed to caregiving in North Carolina. Caregivers describe several barriers to accessing support at the health systems level in Table 1.
Existing Policies and Supports for Caregivers in North Carolina Fall Short
Existing policies and supports for caregivers in North Carolina include providing information on how to access services, offering individual counseling and support groups, caregiver skills training, and respite care.18 An example is the National Family Caregiver Support Program (NFCSP), provided as grants to states.19 The current system is well-intentioned and aligns with needs described by many caregivers, but the system is inadequately funded, variable across counties, and unknown or inaccessible to many caregivers due to restrictive criteria and other limitations. The North Carolina NFCSP provides some support services to caregivers of any age caring for older adults (aged 60 years or older) or caring for a person with Alzheimer’s disease or a related brain disorder. Eligibility also extends to non-parent relatives aged 55 or older raising a related child under age 18, or relatives (including parents) aged 55 or older caring for an adult with a disability.18 This may exclude non-relative caregivers and parental caregivers of children with complex health needs, among others.
The challenges that caregivers face are not adequately addressed by state-level services in three main ways. First, current government programs are inadequate to address the needs of caregivers across the lifespan. Many of these caregivers are at different life stages than those typically considered for existing caregiving programs, interventions, research, and literature. These include youth caregivers, grandparents raising grandchildren, and parents caring for a child with a serious illness or disability. Due to the daily demands of these caregivers—which often include work, school, and other commitments—they may not be able to participate in existing programs and interventions even if they are eligible. In addition, the current systems of care delivery do not fully assess whether caregivers have the skills and capacity to provide needed care, nor do these processes identify and address unmet caregiver needs, such as finding and affording sufficient respite care.
Second, many caregiving programs are currently organized by age and disease state alone, which can be misaligned with the diverse needs and lived experiences of many caregivers and their care recipients. For example, North Carolina is becoming more racially diverse. There are numerous health inequities experienced by Black and Latino/a patients with Alzheimer’s and their caregivers, including higher likelihood of receiving lower-quality care despite higher risk of the disease.20 In addition, a high proportion of North Carolina’s population resides in rural areas,21 and the needs of rural caregivers are often inadequately addressed through existing long-term services and supports administered by the state and federal government.4 These needs include transportation, reliable telecommunications and broadband internet access, and access to health care services. These needs cut across illness types and age and relationship of caregivers and their care recipients. In addition, the focus on age and disease ignores the historic and current inequities of care and disparities across underserved populations.
Finally, caregivers themselves are often unofficial yet essential members of a care recipient’s health care team. However, documentation of caregivers’ needs and roles in care is rare, and systematic, routine collection of basic identifying and demographic information about essential caregivers does not often exist in electronic health records. North Carolina is one of only eight states that has not passed the Caregivers Advise, Record, Enable (CARE) Act. In states that have passed this legislation, hospitals are required to include informal caregivers in communications about care recipient needs for complex care after discharge.22 This lack of caregiver documentation in the health care system hinders surveillance of caregiver health status and its connection to systemic failures to understand the fundamental role of caregivers within health care statewide and beyond.
An Integrated Approach to Caregiving Across the Life Course for All Ages in North Carolina
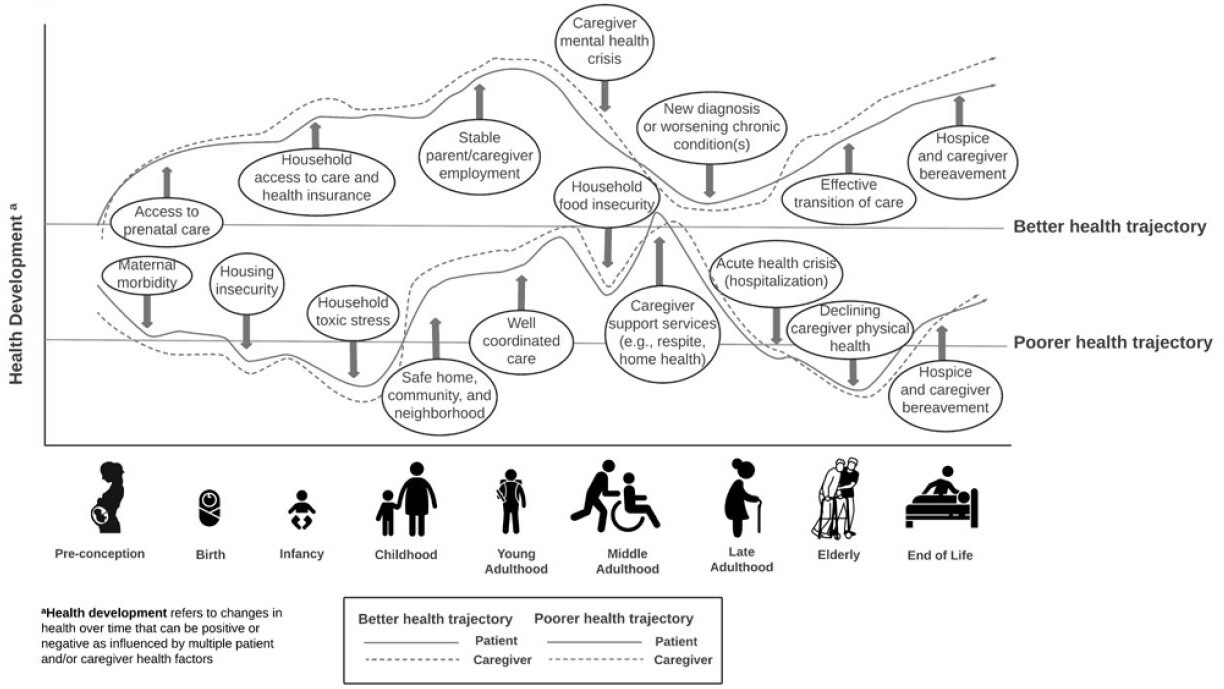
Because caregiving can occur at any life stage and may be short- or long-term, it should be reframed as a life course issue. Life course theory suggests that health care delivery should provide longitudinal supports for managing patients’ and caregivers’ health needs and recognize that these needs are interconnected (Figure 1). In addition, policy development from a life course perspective takes a whole-person, whole-family approach and would provide financial assistance and supports to keep caregivers participating in society. In the case of individuals who require caregiving, their health and the health of their caregiver(s) are intertwined such that the presence of health risk factors and health-promoting factors can have direct—and often compounding—effects simultaneously on caregivers and their care recipients.
The Life Course Health Development (LCHD) framework provides useful guidance relative to caregiving policy. One key tenet of the LCHD framework is that individual health is defined by a core set of assets (i.e., motor function, emotional regulation, cognitive function) that evolve over time.23 At some points in most individuals’ lives, one’s health and their associated core assets will degrade—acutely or chronically—and they will need care from a family member or friend, and/or they will need to assume a caregiver role. This framework illustrates the breadth of caregiving impact across an ever-changing health journey that is not limited to only certain demographic groups (e.g., women in middle age).3
A second key tenet of the LCHD framework is that longitudinal health development cannot be separated from an individual’s dynamic social-environmental conditions. Numerous clinical, social, community, and policy-level factors within the individual patient’s surrounding environment can have a positive or negative impact on overall health trajectories, resulting in nonlinear, variable patterns.24 Understanding how varying health patterns interrelate with multilevel health and environmental factors is essential for development of life course interventions that can improve health and advance health equity.25
The inseparable nature of patient and caregiver health requires a broad framework that can inform systems of care that prioritize and strengthen supports for caregivers.26 A life course perspective informed by the LCHD framework provides a whole-person, whole-family orientation that can guide multilevel decision-making and the implementation of health programs and policies at the individual, family, and societal levels.27 Application of a life course perspective to caregiving can also help to mitigate health disparities by creating a system capable of identifying and addressing common challenges faced by caregivers and their care recipients across the age, race and ethnicity, geographic, and disability spectra. By integrating efforts that support specific populations with serious illness, disabilities, and functional impairment, we can share innovations and center caregiver experiences when designing solutions that address gaps in care and support.28,29
Call to Action
Advocates, researchers, clinicians, care recipients, and caregivers across the state are currently collaborating to create a vision for what caregiver support across the life course might look like in North Carolina. We propose several recommendations to advance support for North Carolina caregivers (Table 2).
The original call to action was issued through the North Carolina Institute of Medicine’s (NCIOM) 2020 report, “Improving Serious Illness Care in North Carolina,” which included a recommendation to establish a task force on caregiving for those with serious illness that can execute the above strategies.5 Since the NCIOM report’s release, the North Carolina Coalition on Aging (COA) and the Children’s Complex Care Coalition of North Carolina (4CNC) have partnered with the North Carolina Serious Illness Coalition (NCSIC) to amplify a united call to action to establish a caregiving task force in North Carolina. A task force is one efficient way to address many of the NCIOM’s recommendations. The task force could analyze additional legislative solutions and financing options to meet caregiver needs.
In addition, the National Alliance for Caregiving has created a blueprint for bringing together state collaboratives and leveraging task forces to promote best practices and strategies for supporting caregivers across state lines.30 For example, the recently established Wisconsin Governor’s Task Force on Caregiving led to the creation of multiple proposals designed to support caregivers, including piloting a tailored caregiver assessment and referral process, creating a caregiving tax credit, and creating a statewide minimum pay band for compensating direct care workers.31 Many of the initiatives and policies recommended in the Wisconsin caregiving task force’s report and underway in other states provide relevant foundations that can serve as a strong starting point and can be tailored to address the needs of caregivers in North Carolina.
Conclusion
The time is now for North Carolina to implement a strategic plan for a comprehensive and longitudinal system of supports for caregivers as their loved ones experience illness, disability, and subsequent complex care needs. At the time of this writing (September 2022), the RAISE Family Caregiving Advisory Council will be introducing the first National Family Caregiving Strategy, including best practices and recommendations for recognizing and supporting family caregivers.32 If action steps are taken now, North Carolina can be well-positioned to align with these national efforts around caregiving supports. Actions should be informed by the perspectives of a diverse range of caregivers at every life stage to ensure representation and mitigate disparities so that North Carolina can truly be a place for health and thriving at all ages. This writing reaffirms the call for a statewide task force to critically examine existing systems and identify strategies to improve support for informal caregivers across health conditions and the life course for all North Carolinians.
Acknowledgments
The authors would like to acknowledge input from members of the North Carolina Serious Illness Coalition, North Carolina Coalition on Aging, and the Children’s Complex Care Coalition of North Carolina.
Disclosure of interests
The authors report no potential conflicts of interest.
Author biographies
Erin E. Kent, PhD, MS associate chair and associate professor, Department of Health Policy and Management, Gillings School of Global Public Health, University of North Carolina at Chapel Hill; member, Lineberger Comprehensive Cancer Center Prevention and Control Program, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Neal A. deJong, MD, MPH associate professor, General Pediatrics and Adolescent Medicine, Department of Pediatrics, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
Harold Barnette cofounder, Institute for Family Caregiving, Inc., Durham, North Carolina.
Sue Deaton, MSN, RN chief engagement officer, Patient Centered Innovation, Inc., Greenville, North Carolina.
Karen Appert, MSG project coordinator, North Carolina Division of Aging and Adult Services, Raleigh, North Carolina.
David Y. Ming, MD associate professor, Departments of Medicine, Pediatrics, and Population Health Sciences, Duke University School of Medicine, Durham, North Carolina.